Thoracentesis: What to Expect
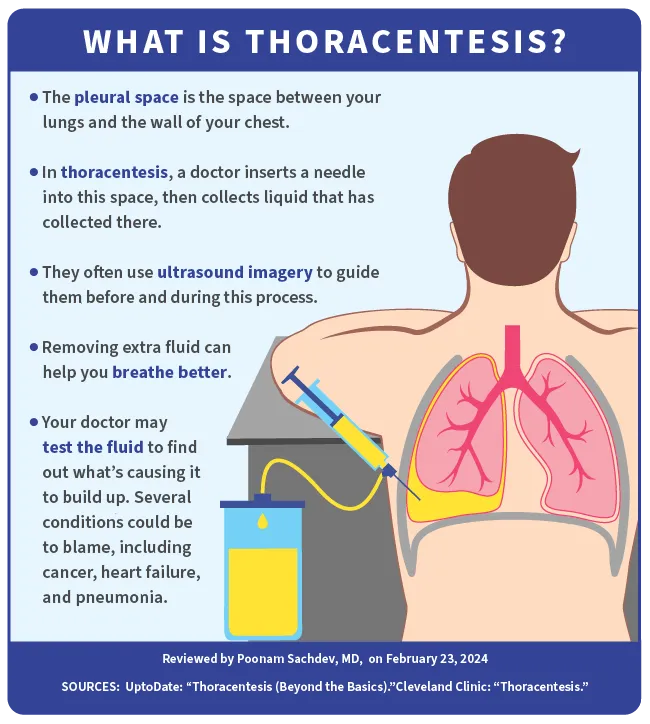
Thoracentesis is a procedure in which a doctor uses a needle and catheter to remove excess fluid from the space between your lungs and the wall of your chest, known as the pleural space. You might also hear this procedure called thoracocentesis, pleural aspiration, or pleural tap.
Normally, there are about 4 teaspoons of fluid in this area. It helps keep the membranes surrounding your lungs (the pleura) from rubbing together as you breathe. But certain health conditions can cause a fluid buildup, a condition called pleural effusion. This puts extra pressure on your lungs and makes it harder to breathe.
Doctors do thoracentesis to both remove the excess fluid and find out what's causing it. They often use ultrasound imaging to guide them as they insert the needle through your chest wall and into the pleural space. Depending on how serious your condition is, this can be a short, outpatient procedure.
Thoracentesis Indications
Removing excess fluid from the pleural space eases shortness of breath, chest pain, and pressure on your lungs. And lab tests on the fluid that's removed can help pinpoint the reason behind the buildup. The most common cause is congestive heart failure, which is when your heart doesn’t properly pump out blood to your body.
Other conditions that might cause pleural effusion include:
- An area of pus in the pleural space (called an "empyema")
- A b lood clot in the lung
- Cancer
- High blood pressure in the lung blood vessels (pulmonary hypertension)
- Liver failure
- Pneumonia
- Reactions to medicine
- Tuberculosis
- Viral, fungal, or bacterial infections
Thoracentesis Preparation
In addition to your doctor's instructions, keep the following in mind:
- Your doctor will take your blood pressure and measure your blood oxygen level before doing a thoracentesis.
- You may also have a blood test before the procedure. This can show how your kidneys are doing and whether your blood clots normally.
- Tell your doctor if you have a history of bleeding problems.
- Make a list of all medications and supplements you take, including over-the-counter ones. Make sure to tell your doctor if you take aspirin, blood thinners, or anything else that could lead to bleeding. You may need to stop taking certain medications before the procedure.
- Inform your doctor about any allergies you have, including those to latex, tape, or anesthesia (medication that stops you from feeling pain).
- Let your doctor know if you think you may be pregnant.
- You'll need to wear a hospital gown and remove any jewelry you're wearing.
- Your doctor may want you to arrange for someone to drive you home. You may be groggy from the medicine given to you to numb pain during the procedure.
Thoracentesis Procedure
You'll likely have an imaging scan, such as an ultrasound or chest X-ray, before thoracentesis to show your doctor exactly where the fluid is. From there, most cases happen this way:
- The best thoracentesis position is sitting on a chair or bed with your arms resting on a table. This spreads out the space between your ribs.
- The area where your doctor will do the procedure is cleaned and numbed. Sometimes, younger children are given medicine that makes them sleepy.
- The doctor will insert the needle between the ribs in your back. Often, doctors use ultrasound imagery to guide them during this process.
- They'll attach a catheter (tube) to the needle and withdraw the fluid into it. You may feel some pressure, but it shouldn't hurt.
- The doctor may ask you to be still, exhale, or hold your breath at different times.
- Once enough fluid has been drained, they'll remove the needle, and the area will be bandaged. The spot where the needle went in will close without any stitches.
- When the procedure is complete, your doctor may do another ultrasound or X-ray to check your lungs.
Thoracentesis usually takes about 15 minutes. It may take longer if there's a lot of fluid to remove.
Thoracentesis Post-Op Care
After the procedure, a nurse will closely watch your blood pressure, pulse, and breathing. Your bandage may also be checked before you're released.
You may cough a lot for up to an hour afterward as your lungs re-expand.
When you get home, follow your doctor's directions for diet and physical activity . Call them if you have any of these symptoms:
- A fever of 100.4 F or higher
- Redness, swelling, and blood or other fluid leaking from the injection site
- Breathing issues or chest pain
Your doctor's office will send samples of your pleural fluid to a lab for testing and let you know about the results.
Thoracentesis Complications
Any medical procedure has some risks. Though thoracentesis is generally considered safe, you could have complications such as:
- Pulmonary edema, or fluid in the lungs
- Pneumothorax, or collapsed lung
- Infection at the site where the needle pierced your skin
- Liver or spleen injury (this is rare)
Thoracentesis Results
Several tests are usually done on the fluid taken during your thoracentesis. This is called pleural fluid analysis. It can show your doctor what type of fluid is in your pleural space:
Transudate is a watery fluid with low levels of protein. It results when pressure in the blood vessels causes fluid to leak into your pleural space. It's often an indication of:
- Heart failure
- Kidney disease
- Liver disease, such as cirrhosis
Exudate is a cloudy fluid containing high levels of protein. It may result from infections, inflammation, and conditions that involve your immune system or blood vessels, such as:
- Autoimmune conditions such as lupus and rheumatoid arthritis
- Cancer
- Lung diseases such as pneumonia, or a lung injury
- Pancreatitis
Exudate can give further clues to your condition because it may contain other substances, such as blood, cancer cells, or bacteria.
Your doctor may order further tests on your fluid sample to check for certain substances, depending on what they think may be causing the pleural effusion. You might also need other tests such as blood or pee tests, a biopsy, or a bronchoscopy.
After evaluating the findings, as well as your symptoms and medical history, your doctor will let you know the results and come up with a treatment plan.
Takeaways
Thoracentesis is a brief, nonsurgical procedure in which a doctor drains excess fluid that collects in the space between your chest and lungs. It eases the chest pressure this extra fluid causes. It also provides a sample of the fluid, which can be tested to help your doctor determine what's causing the fluid buildup.
Thoracentesis FAQs
How long does it take to recover from thoracentesis?
You may need to avoid strenuous activity for a couple of days. But you can resume your normal daily activities as soon as you feel you're able to do so. Your bandage can come off in 24 hours.
Are you awake during thoracentesis?
You'll be awake during this short procedure. Your doctor will use a local anesthetic to numb the area where they'll give the injection.
How bad does a thoracentesis hurt?
It might sting a little when your doctor injects the local anesthetic. And you may feel some pressure and discomfort while your doctor puts the needle into your pleural space. But the local anesthesia will make the area numb, so the procedure shouldn't be painful.
