- Overview
- Symptoms
- Causes & Risks
- Tests & Diagnosis
- Treatment
- Living With
- Complications
- View Full Guide
A Visual Guide to Psoriatic Arthritis

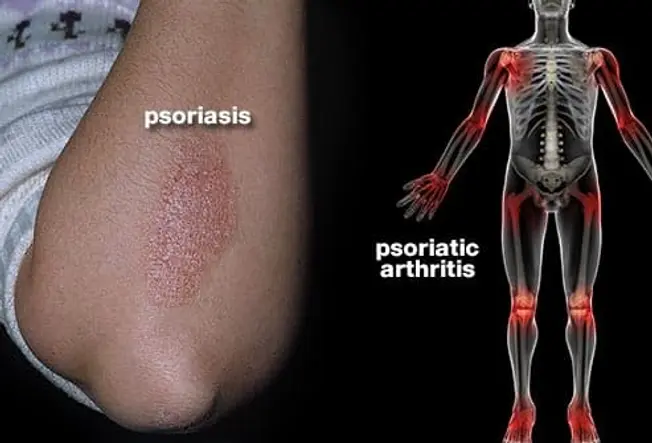
What Is It?
When you have psoriasis -- a condition that makes thick patches of itchy red, white, or silvery skin -- you could get psoriatic arthritis, too. The inflammation of your skin comes from your body's immune system going haywire. Your immune system might also attack your joints, making them swollen and stiff. An early diagnosis can prevent or limit the damage.
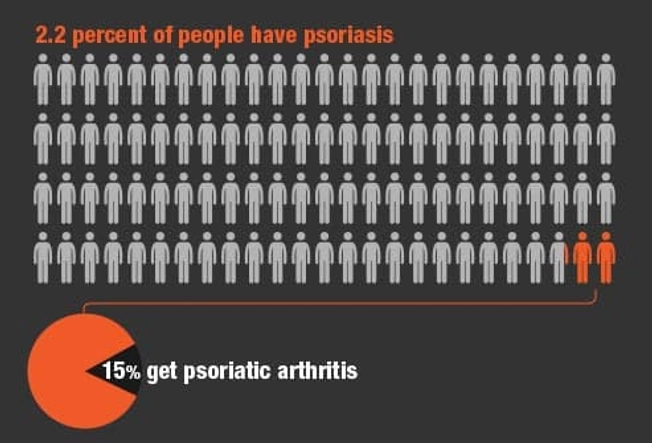
Who Gets It?
Most people who get psoriatic arthritis already have psoriasis. Only about 15% get it without any history of skin trouble.
If you have psoriasis and you notice joint pain, see a doctor who specializes in arthritis. Up to 3 in 10 people who have psoriasis get psoriatic arthritis.

Causes
We don't know exactly what causes it. It's most likely passed on in families. About 40% of people with the condition have a close relative who has joint or skin problems, too. Infections like strep throat may also have some links to psoriasis.

Warning Signs
Stiff, puffy, sausage-like fingers or toes are common, along with joint pain and tenderness. The psoriasis flares and arthritis pain can happen at the same time and in the same place, but not always. You may also notice:
- Dry, red skin patches with silvery-white scales
- Tiny dents in your nails
- Nails that separate from the bed
- Fatigue
- Eye redness and pain
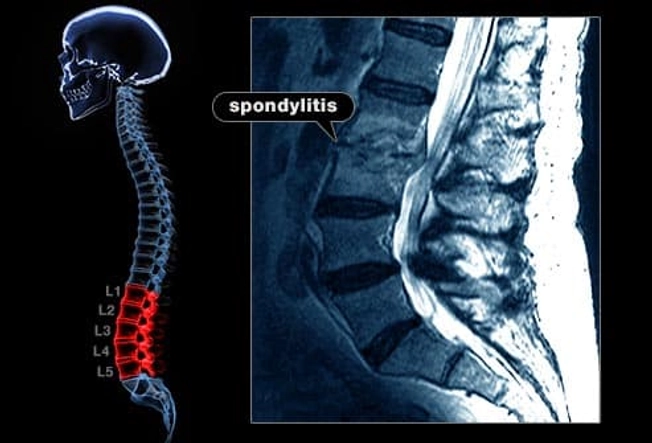
Back and Heel Pain
One form of psoriatic arthritis can inflame the joints in and near your spine. It's called spondylitis, and it causes back and neck pain.
Another form causes pain, tenderness, or swelling where tendons attach to your bones, like in your heel. It can also affect your hands, knees, hips, and chest.

Diagnosis
An arthritis specialist called a rheumatologist can diagnose psoriatic arthritis and recommend a treatment. They'll look at your joints and skin for any swelling, pain, or nail changes. Your doctor may also order X-rays, MRIs, ultrasounds, or CT scans to check for joint damage. Blood, joint fluid, and skin samples can rule out other forms of arthritis.

Treatment
If your arthritis is mild, you might only need an over-the-counter medicine with ibuprofen or naproxen when your joints are sore. A corticosteroid shot into a joint can lessen heat, swelling, and pain. Prescription drugs called DMARDs (disease-modifying antirheumatic drugs) relieve severe symptoms. They slow or stop psoriatic arthritis from getting worse and can ease skin problems. Your doctor may suggest other things to treat your psoriasis, too.

Biologic Medicines
Biologics target parts of your immune system. They can slow down damage to your joints and ease symptoms like joint pain, swelling, and scaly skin. Your doctor may prescribe one for you when other drugs aren't working.

Ease Pain
Try heat and cold to relieve pain. Soak in a warm bath, take a shower, or use a hot pack to relax your aching muscles and relieve soreness. Apply a bag of ice or frozen vegetables wrapped in a towel to numb a joint and relieve swelling.

Exercise
Pain and swelling get worse when you're not active. Swimming and walking in a pool are good no-impact cardio workouts that ease pain and also build strength and flexibility. (Shower right after you get out of the pool so the chlorine doesn't dry your skin.)
If you're not sure how to get moving safely, a physical therapist can help.

Beat Fatigue
Regular exercise can also boost your energy and help you sleep better at night. Pain medication helps, too.
Get up later in the morning, or take an afternoon nap. Save your energy for things that are most important or that you enjoy most. It's OK to ask family or friends to lend a hand.

Living Well
About a third of people with psoriatic arthritis have a mild form that doesn't change over time. Others need long-term treatment for their symptoms. Even severe psoriatic arthritis doesn't have to be disabling, though. Pro golfer Phil Mickelson (a spokesman for the drug Enbrel) credits an early diagnosis and good treatment with helping him overcome near-crippling pain to stay in the game.