What Is Ductal Carcinoma?
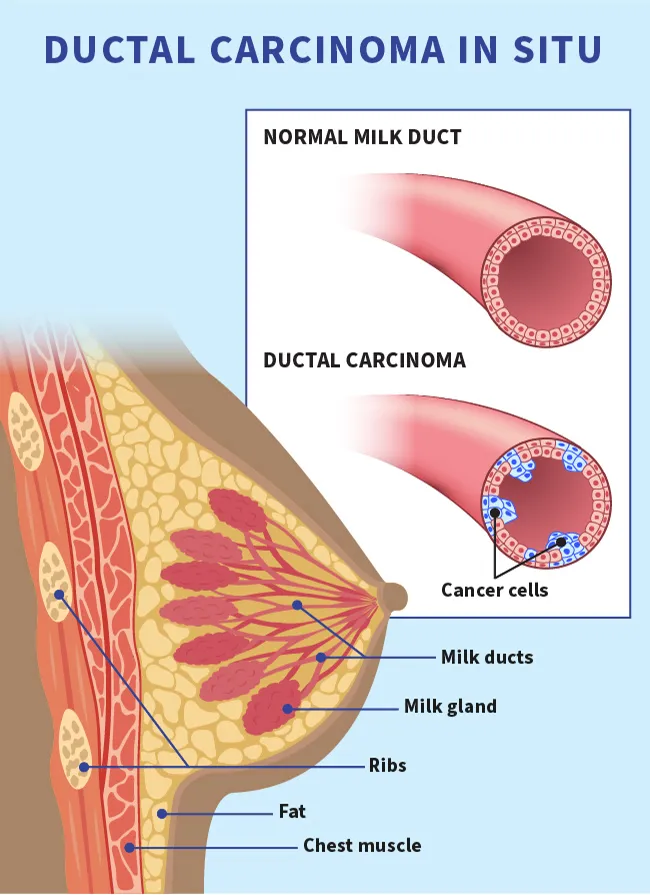
Ductal carcinoma is a common type of breast cancer that starts in cells that line the milk ducts, which carry breast milk to the nipple.
There are two types:
- Invasive ductal carcinoma (IDC)
- Ductal carcinoma in situ (DCIS), also called intraductal carcinoma
The symptoms, diagnosis, and treatments for each are different.
What Is Invasive Ductal Carcinoma?
Invasive (or infiltrating) ductal carcinoma (IDC) accounts for about 80% of all invasive breast cancers.
It begins in the cells of a milk duct, then it grows through the duct walls and into the surrounding breast tissue. It can also spread to other parts of your body.
IDC causes and risk factors
It’s not known exactly what causes each case of breast cancer. But we do know many of the risk factors for these cancers, including lifestyle, hormones, and family history. Normal breast cells can become cancerous because of changes (or mutations) in genes. But only about 1 in 10 breast cancers (10%) are linked with known abnormal genes that are inherited or passed on from parents. Most breast cancers (about 90%) develop from acquired (not inherited) gene changes that have not yet been identified. Risk factors for IDC and other breast cancers include:
- Certain inherited gene mutations, such as the BRCA1 and BRCA2 breast cancer gene mutation
- A family history of breast cancer
- A personal history of breast cancer or benign (non-cancerous) breast conditions
- Being born female
- Aging (over 55 years)
- Being taller
- Having dense breast tissue
- Race and ethnicity – breast cancer is slightly more common in White women, but in women under age 40, it’s more common in Black women. Asian, Hispanic, and Native American women have a lower risk.
- Having your first menstrual period before age 12
- Beginning menopause after age 55
- Having had radiation therapy to your chest as a teen or young adult (under 40)
- Exposure to an estrogen-like drug called diethylstilbestrol (DES)
- Drinking alcohol
- Being overweight or obese
- Being physically inactive
- Giving birth after age 30 or never having a child
- Birth control methods that involve hormones
- Menopausal hormone therapy
- Smoking
Symptoms of Invasive Ductal Carcinoma
Invasive ductal carcinoma symptoms include:
- A lump in your breast
- Thickened breast skin
- A rash or redness on your breast
- Swelling or changes to the shape of your breast
- New pain in your breast
- Dimpling on your breast (also called peau d’orange, which means orange peel) or the skin of your nipple
- Nipple pain
- An inverted nipple
- Nipple discharge (other than breast milk)
- Flaky skin on the nipple or a sore on the breast or nipple (possibly a sign of Paget’s disease, another type of breast cancer that can occur along with IDC)
- Lumps under your arm
- Changes to your breast or nipple that are different from the ones you have with your period
Invasive Ductal Carcinoma Diagnosis
IDC is usually found as the result of an abnormal mammogram. It may be detected during a physical exam when a lump or thickening is felt in the breast. IDC can also be discovered during a breast ultrasound, which uses sound waves to create a computerized image of breast tissue and blood flow. People with dense breast tissue sometimes have regular ultrasounds instead of, or in addition to, mammograms. An ultrasound may also be ordered after a concerning or abnormal mammogram.
To diagnose cancer, you’ll get a biopsy to collect cells for analysis. The doctor will remove a bit of tissue to look at under a microscope. They can make a diagnosis from the biopsy results.
If the biopsy confirms you have cancer, you’ll likely have more tests to see how large the tumor is and if it has spread:
- CT scan. It's a powerful X-ray that makes detailed pictures inside your body.
- PET scan. The doctor injects a radioactive substance called a tracer into your arm. It travels through your body and gets absorbed into the cancer cells. Together with a CT scan, this test can help find cancer in lymph nodes and other areas.
- MRI. It uses strong magnets and radio waves to make pictures of the breast and other structures inside your body.
- Bone scan. The doctor injects a tracer into your arm. They take pictures to find out if cancer has traveled to your bones.
- Chest X-ray. It uses low doses of radiation to make pictures of the inside of your chest.
Invasive Ductal Carcinoma Stages
Results from these tests will show the stage of your cancer. Staging is the name for the process doctors use to figure out if and how far breast cancer has spread. Knowing the stage will help guide your treatment.
Doctors can use the results from your diagnostic testing to gather information about the tumor. They group it by a system known as TNM:
- Tumor (T): How large is the primary tumor? Where is it?
- Node (N): Has the tumor spread to your lymph nodes? Where? How much?
- Metastasis (M): Has the cancer spread to other body parts? Which ones? How much?
To stage your cancer, your doctor combines the TNM results with the tumor grade (how your tumor cells and tissue look under a microscope), your hormone receptor status (if the cancer cells have proteins that respond to the hormones estrogen or progesterone), and your HER2 status (whether your cancer is affected by the HER2 gene).
Stages include:
- Stage 0: This is noninvasive cancer. It’s only in the ducts and hasn’t spread (N0, M0).
- Stage IA: The tumor is small and invasive, but it hasn’t spread to your lymph nodes (T1, N0, M0).
- Stage IB: Cancer has spread to the lymph nodes. It’s larger than 0.2 millimeters but less than 2 millimeters in size. There’s either no sign of a tumor in the breast, or there is but it’s 20 millimeters or smaller (T0 or T1, N1, M0).
- Stage IIA: Any one of these:
- There’s no sign of a tumor in the breast. The cancer has spread to between one and three underarm lymph nodes, but not to any distant body parts (T0, N1, M0).
- The tumor is 20 millimeters or smaller and has spread to underarm lymph nodes (T1, N1, M0).
- The tumor is between 20 millimeters and 50 millimeters but hasn’t spread to nearby nodes (T2, N0, M0).
- Stage IIB: Either of these conditions:
- The tumor is between 20 millimeters and 50 millimeters and has spread to one to three underarm lymph nodes (T2, N1, M0).
- The tumor is larger than 50 millimeters but hasn’t spread to underarm lymph nodes (T3, N0, M0).
- Stage IIIA: Either of these conditions:
- Cancer of any size has spread to four to nine underarm lymph nodes or those under your chest wall. It hasn’t spread to other body parts (T0, T1, T2 or T3, N2, M0).
- A tumor larger than 50 millimeters has spread to one to three nearby lymph nodes (T3, N1, M0).
- Stage IIIB: The tumor:
- Has spread to the chest wall
- Has caused swelling or breast sores
- Has been diagnosed as inflammatory breast cancer
- May or may not have spread to up to nine lymph nodes under your arm or beneath the chest wall
- Hasn’t spread to other body parts (T4; N0, N1 or N2; M0)
- Stage IIIC: A tumor of any size that has spread to 10 or more nearby lymph nodes, breast lymph nodes, and/or lymph nodes under the collarbone. It hasn’t spread to other body parts (any T, N3, M0).
- Stage IV (metastatic): The tumor can be any size and has spread to other organs, like your bones, lungs, brain, liver, distant lymph nodes, or chest wall (any T, any N, M1). Between 5% and 6% of the time, metastatic cancer is discovered upon first diagnosis. Your doctor may call this de novo metastatic breast cancer. More often, it’s found after a previous diagnosis of early breast cancer.
- Recurrent: This is cancer that comes back after treatment. It can be local, regional, and/or distant. If your cancer returns, you’ll get another round of tests to learn about the extent of the recurrence. They’ll be similar to those at your original diagnosis.
Invasive Ductal Carcinoma Treatment
Most people with IDC have surgery to remove the cancer. The treatment options are usually:
- Lumpectomy. The surgeon only removes the tumor and a bit of the tissue around it to help make sure all the cancer cells have been removed. You might hear it called breast-conserving surgery
- Mastectomy. The surgeon removes an entire breast. This may be followed by breast reconstruction (surgery to re-create the shape of a breast).
- Lymph node dissection and removal. To find out if the breast cancer has spread, the surgeon will remove one or more underarm (axillary) lymph nodes so they can be examined in the lab. This helps the doctor determine the stage of the cancer (how big it is and where it has spread). This may be done during the same surgery to remove the tumor or as a separate operation.
Which treatment you get depends on the size of your tumor and how much it has spread throughout your breast and surrounding lymph nodes.
In addition to surgery, other treatments may include:
- Radiation. This usually follows your surgery.
- Hormone therapy. You’ll get it if your cancer is hormone receptor-positive (meaning estrogen helps it grow). These drugs block or lower the amount of estrogen in your body.
- Chemotherapy. These medications target cancer cells throughout your body. Doctors may also use It before surgery to shrink tumors and after to kill any cancer cells left behind.
- Targeted therapy. These medications block cancer cell growth. You might get them along with chemotherapy.
- Immunotherapy. These medications help your own immune system recognize and destroy cancer cells better.
You might get one treatment or a combination.
Side effects of IDC treatment
While breast cancer treatment is necessary and helpful in most cases, each kind of treatment can cause short-term and long-term side effects. Your health care team may be able to help you manage many of these side effects.
Side effects of surgery may include:
- Blood clots
- Infected surgical site
- Buildup of fluid (seroma) at the surgical site
- Buildup of blood (hematoma) at the surgical site
- Pain, discomfort, numbness, or tingling
- Stiffness
- Swelling
- Nerve pain
- Fatigue (extreme tiredness)
- A change in sensation around the surgical site
- Scar tissue at the surgical site
- Bruising and other skin changes
- Nausea
- Hardening of lymph nodes from the armpit down the arm (cording)
- Lymphedema (long-term swelling of the arms and other areas caused by removal of lymph nodes)
Side effects of chemotherapy and targeted therapy may include:
- Hair loss
- Mouth sores
- Fatigue (extreme tiredness)
- Loss of appetite
- Nausea and vomiting
- Diarrhea
- Nail changes
- Bruising
- Pain, tingling, or numbness (neuropathy) in the hands and feet
- A hard time focusing or remembering (“chemo brain”)
- A higher risk of infection from having a lower immune system
- Hormone-related problems such as vaginal dryness, hot flashes, early menopause, fertility issues, or a low white or red blood cell count
- Cardiac (heart) changes
- Rashes and/or dry skin
Side effects of radiation therapy may include:
- Fatigue (extreme tiredness)
- Breast tenderness
- Swelling or skin irritation (redness, pain, peeling) at the radiation site
Side effects of hormone therapy may include:
- Hot flashes
- Vaginal dryness
- Night sweats
- Muscle and joint pain
- Osteoporosis (loss of bone density)
- Weight gain
- Headaches
- Nausea
- Fatigue (extreme tiredness)
- Mood swings
- Low sexual desire
- Changes in your menstrual cycle or early menopause
IDC treatment recovery
Your recovery time from treatment for invasive ductal carcinoma will depend on the specific procedures you had, your overall health and fitness level, and any side effects or complications you may have had.
After breast surgery, you may feel tired and sore for several weeks. You may need to do arm and shoulder exercises to prevent stiffness and help with movement. Most people are able to get back to normal activities after a month.
Chemotherapy is usually scheduled so your body has time to recover between treatments. Some side effects from chemotherapy will go away when treatment is finished. Others may last for months or years, though this happens more rarely and there are often medicines or therapies that can help.
Invasive Ductal Carcinoma Survival Rates
The American Cancer Society's 5-year survival rates for breast cancer in the United States are based on how far the cancer has spread:
- Localized IDC, meaning the cancer has not spread outside the breast: nearly 100%
- Regional IDC, meaning the cancer has spread outside the breast to nearby tissue or lymph nodes: 86%
- Distant IDC, meaning the cancer has spread to distant parts of the body like the liver, lungs, or bones: 31%
What Is Ductal Carcinoma in Situ (DCIS)?
Ductal carcinoma in situ (DCIS), also known as intraductal carcinoma, accounts for 1 of every 5 new breast cancer diagnoses. It's an uncontrolled growth of cells within the breast ducts. It’s noninvasive, meaning it hasn’t grown into the breast tissue outside of the ducts. The phrase "in situ" means "in its original place."
DCIS is the earliest stage at which breast cancer can be diagnosed. It's known as stage 0 breast cancer. The vast majority of people diagnosed with it can be cured.
Even though it’s noninvasive, it can lead to invasive cancer. It's important that those with the disease get treatment. Research shows that the risk of getting invasive cancer is low if you’ve been treated for DCIS. If it isn’t treated, 30% to 50% of those with DCIS will get invasive cancer. The invasive cancer usually develops in the same breast and in the same area where the DCIS happened.
DCIS Symptoms
DCIS usually has no symptoms. Most of the time, it’s found by a mammogram and appears as small white clusters (calcifications) in odd shapes and sizes. DCIS can sometimes cause these symptoms:
- A breast lump
- Bloody nipple discharge
- Itchy skin
DCIS Diagnosis
About 80% of cases are found by mammograms. On the mammogram, it appears as a shadowy area.
If your mammogram suggests that you may have DCIS, your doctor should order a biopsy to analyze the cells and confirm the diagnosis. Biopsies for DCIS are typically done using needles to remove tissue samples from the breast.
If you have DCIS, your doctor may do more tests to gather information about your cancer. These tests may include an ultrasound or MRI. Based on the results of various tests, your doctor will be able to tell the size of your tumor and how much of your breast is affected by the cancer.
DCIS Treatment
Your doctor will customize your treatment plan based on your test results and medical history. Among other things, your doctor will consider:
- Tumor location
- Tumor size
- Aggressiveness of the cancer cells
- Your family history of breast cancer
- Results of tests for a gene mutation that would increase the risk of breast cancer
Most people with DCIS don't have the breast removed with a mastectomy. Instead, they have a lumpectomy.
Most common is a lumpectomy followed by radiation. The surgeon removes the cancer and a small area of healthy tissue around it. Lymph nodes under the arm don’t need to be removed as they are with other types of breast cancer.
After a lumpectomy, radiation cuts the chances that the cancer will come back. If cancer does return, it’s called recurrence.
Some people may opt to have a lumpectomy only. Discuss the risks of not having radiation with your doctor before deciding against it.
You and your doctors may decide that a mastectomy to remove the breast is the best course of treatment if you have any of the following:
- A strong family history of breast cancer
- A gene mutation that makes having breast cancer more likely
- A very large areas of DCIS
- DCIS lesions in multiple areas throughout your breast
- Not being able to tolerate radiation therapy
You and your treatment team may also consider the use of hormone therapy if the cancer tests positive for hormone receptors (HR+ breast cancer). Hormone therapy is a treatment to block hormones from reaching cancer cells and can cut the chance of getting another breast cancer in either breast.
Hormone therapy is considered an additional (adjuvant) treatment to be given after surgery or radiation. The drug tamoxifen can be taken for up to 5 years to reduce your risk of having invasive breast cancer, whether you are premenopausal or postmenopausal. If you're postmenopausal, you may also be offered hormone therapy with medicines called aromatase inhibitors. These drugs reduce the amount of estrogen your body produces and can be taken for up to 5 years.
Side effects of DCIS treatment
Side effects of surgery may include:
- Blood clots
- Infected surgical site
- Buildup of fluid (seroma) at the surgical site
- Buildup of blood (hematoma) at the surgical site
- Pain, discomfort, numbness, or tingling
- Stiffness
- Swelling
- Nerve pain
- Fatigue (extreme tiredness)
- A change in sensation around the surgical site
- Scar tissue at the surgical site
- Bruising and other skin changes
- Nausea
Side effects of radiation therapy may include:
- Fatigue (extreme tiredness)
- Breast tenderness
- Swelling or skin irritation (redness, pain, peeling) at the radiation site
Side effects of hormone therapy may include:
- Hot flashes
- Vaginal dryness
- Night sweats
- Muscle and joint pain
- Osteoporosis (loss of bone density)
- Weight gain
- Headaches
- Nausea
- Fatigue (extreme tiredness)
- Mood swings
- Low sexual desire
- Changes in your menstrual cycle or early menopause
DCIS treatment recovery
Your recovery time from treatment for ductal carcinoma in situ will depend on the procedures you had, your overall health and fitness level, and any side effects or complications you may have had.
After breast surgery, you may feel tired and sore for several weeks. You may need to do arm and shoulder exercises to prevent stiffness and help with movement. Most people are able to get back to normal activities after a month.
Ductal Carcinoma Prevention
Some risk factors for breast cancer, such as your family history, can’t be changed. But there are lifestyle choices you can make to help lower your risk of getting breast cancer. These include:
- Limiting or avoiding alcohol
- Maintaining a healthy weight
- Staying active – aim for 150 minutes a week of cardio (such as walking, biking, or running) and strength training at least twice a week
- Quitting smoking
- Eating a healthy diet (such as the Mediterranean diet)
- Breastfeeding after having a baby
- Discussing your family history with your doctor and, if recommended, having genetic testing
- Limiting hormone replacement therapy after menopause (This is different from hormone therapy used after breast cancer.)
- Chemoprevention – taking medication such as tamoxifen and aromatase inhibitors to prevent hormone receptor-positive breast cancers
Takeaways
Invasive ductal carcinoma (IDC), the most common type of breast cancer in the U.S., starts in your milk ducts and spreads to nearby tissue. Like IDC, ductal carcinoma in situ (DCIS) starts in your milk ducts, but it does not spread outside the duct walls. Treatment for IDC and DCIS may include a combination of surgery, radiation therapy, chemotherapy, hormone therapy, or other medications.
Ductal Carcinoma FAQs
How serious is invasive ductal carcinoma?
Invasive ductal carcinoma (IDC) starts in your milk ducts and spreads to your surrounding breast tissues. Eventually, it can spread (metastasize) to your lymph nodes and other areas of your body. IDC is serious and should be treated to remove the cancer and reduce the chance of it coming back (recurring). When IDC is detected and treated early (before it spreads beyond the breast), it has a high survival rate.
What is early-stage invasive breast cancer?
Stage I breast cancer is the earliest stage of invasive breast cancer (meaning the cancer has spread to other areas of the body beyond where it started). In stage I breast cancer, cancerous cells have spread to the surrounding normal tissue or lymph nodes and is usually contained to a small area. Stage I invasive breast cancer is classified into two categories:
- In stage IA breast cancer, the tumor is smaller than 20 millimeters and has not spread to the lymph nodes.
- In stage IB breast cancer, there are cancerous cells in the lymph nodes. There is usually also a small cancerous tumor (20 millimeters or smaller) in the breast, though sometimes the cancer is only in the lymph nodes.
Stage I breast cancer is considered early-stage, localized cancer and is highly treatable and survivable.
What is the most invasive type of breast cancer?
While invasive ductal carcinoma (IDC) is the most common form of invasive breast cancer, responsible for 80% of all cases in the U.S., it is not the most aggressive. Triple-negative breast cancers tend to grow and spread more quickly than other types. A breast cancer is considered triple negative if it tests negative for three receptors (proteins) known to fuel breast cancer growth: estrogen (ER) and progesterone (PR) hormone receptors and human epidermal growth factor receptor 2 (HER2).
Do you need chemo for invasive ductal carcinoma?
The treatment your doctor will recommend for IDC will depend on the size and location of your tumor, your personal and family medical history, the type of cancer you have (hormone receptive, for example), and other factors. You may need chemotherapy before surgery to shrink the tumor or after surgery to reduce the chance of cancer returning. Chemotherapy may also be recommended as the main treatment for people with breast cancer that has spread to other parts of the body (metastatic cancer).
Do you need chemo for ductal carcinoma in situ?
DCIS is considered a noninvasive or pre-invasive breast cancer. Because the cancer cells haven’t spread beyond the walls of your milk ducts, chemotherapy is not typically recommended. Surgery and radiation therapy are the most common treatments and may be followed by hormone therapy, if appropriate.
Do I need a mastectomy for DCIS?
You may need a mastectomy (removal of the entire affected breast or both breasts) if breast-conserving surgery (BCS) or lumpectomy is not enough. (For example, if the cancer is very large or has spread to multiple milk ducts.) If you have a mastectomy, you will probably not need radiation therapy.

