Pancoast tumors form at the very top of either lung. They are usually non-small cell lung cancers. Because of their location, they frequently invade adjoining tissue.
Pancoast tumors form an abnormal patch of tissue over the lung apex and principally involve the chest wall structures rather than the underlying lung tissue. They may invade areas such as lymph nodes, nerves, ribs, and spine.
Pancoast Tumor Causes
The risk factors for almost all lung cancers are similar. These include the following:
Pancoast Tumor Symptoms
Although a Pancoast tumor is a lung tumor, it rarely causes symptoms that are typically related to the lungs (like cough or shortness of breath).
The initial symptom is usually pain in the shoulder, the inner part of the shoulder blades, or both.
The pain may later extend to the inner side of the arm, the elbow, as well as the pinky and ring fingers.
The associated pain is severe and constant, often requiring narcotic pain medications for relief. The affected person usually needs to support the elbow of the affected arm in the opposite hand to ease the tension on the shoulder and upper arm.
The hand, arm, and forearm may weaken, muscles degenerate or shrink from disuse, or develop a sensation of pricking, tingling, or creeping on the skin.
If the tumor extends to the certain nerves, Horner syndrome may develop on one side of the face. Horner syndrome is characterized by a drooping eyelid, absence of sweating on the affected side of the face, and narrowing of the pupil.
In up to 25% of people with a Pancoast tumor, compression of the spinal cord and paralysis of the lower half of the body develop when the tumor extends into the opening between two vertebrae.
Pancoast Tumor Exams and Tests
Exams and tests that may be used to diagnose a Pancoast tumor include:
- Chest X-ray
- In the early stages, Pancoast tumors are difficult to detect on chest X-rays because the top of the lung is located in an area of the body that is difficult to visualize clearly on an X-ray. Shadows that lie over the lungs make the image on the X-ray film unclear. Many patients end up consulting orthopedic surgeons and/or neurologists before a definitive diagnosis is made.
- A chest X-ray may reveal anything from asymmetry of the top of the lungs in the form of a small, uniform patch of tissue on the apex of one lung to a large mass, depending on the stage when the tumor is first diagnosed.
- The plain chest X-ray may show that the tumor has invaded one or more ribs or parts of the vertebrae. Bone destruction of the back ribs may be visible on the X-ray.
- CT scan of the chest: A CT scan helps determine if the tumor has invaded areas such as the trachea (windpipe) or esophagus (food pipe). Contrast CT scanning, with the help of an injected, radioactive dye that is visible on the scan, is useful for assessing if the tumor has involved the blood vessels under the collarbone.
- MRI of the chest: MRI findings are more accurate than CT scans in identifying the extent of the tumor's growth. An MRI can also better assess the tumor's invasion of nearby areas.
- Arteriogram or venogram: For this test, a liquid is injected into nearby blood vessels so they will show up on an X-ray. Rarely, a Pancoast tumor involves the artery or the vein under the collarbone.
- Bronchoscopy (using a tubular, illuminated instrument for inspecting the airways of the lung) helps evaluate the tracheal and bronchial cavities. However, because most Pancoast tumors form on the periphery of the lung, bronchoscopy does not usually help the doctor make a diagnosis.
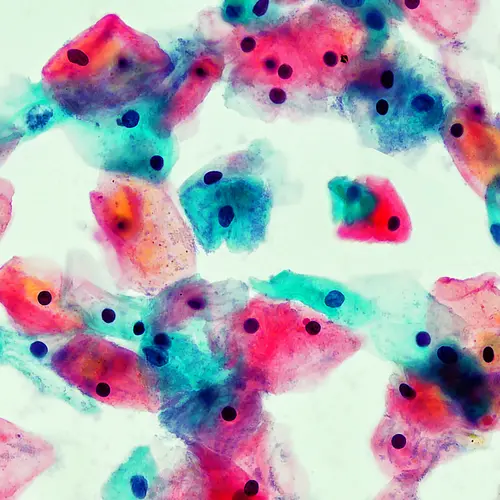
- Biopsy: This is the removal of a sample of tissue for examination under a microscope. Following a needle biopsy, the doctor can make a diagnosis in 95% of people with a Pancoast tumor based on results from the biopsy, either with the help of an X-ray or CT scan to help guide the doctor.
- Although more than 90% of patients can be correctly diagnosed based on clinical and radiological findings (chest X-ray, CT, MRI) alone, open biopsy of the tumor for confirmation may need to be performed through an incision above the collarbone. A definite diagnosis is important before proceeding with treatment of a Pancoast tumor. Results from a needle biopsy are also useful in determining the cell type prior to treatment. Even though getting a diagnosis is relatively simple, performing a tissue biopsy is almost always necessary.
Tests to Determine Spread
- Among other considerations, a CT or MRI scan of the brain is usually recommended in the initial evaluation, because distant spread to the brain is common, and diagnosis of these is necessary to determine treatment.
Mediastinoscopy: This procedure is performed to determine the extent the tumor has spread into nearby areas. It is a procedure in which a tube is inserted behind the breastbone through a small cut at the lowest part of the neck. Samples of lymph nodes are taken from this area to look for cancer cells.
Positron emission tomography (PET) scans (a nuclear imaging technique used to view body functions) may help identify involved lymph nodes and the distant spread of cancer. - Bone scans may be used to see if the cancer has spread to the bones.
Treatment for a Pancoast Tumor
Medical management plays a large role in the treatment of Pancoast tumors. If the cancer has spread, medical treatment is required to reduce the symptoms without curing the underlying cause.
Medications for Pancoast Tumors
The standard of care for people with a Pancoast tumor is chemotherapy and radiation followed by removal of the tumor and a portion of the the chest wall if it is affected or if its removal facilitates surgery. The purpose of the chemotherapy and radiation is to shrink the tumor and to block the cancer from spreading through lymph nodes. An interval of two to four weeks after the chemo and radiation allows the procedures to reach their maximal effect. After four weeks, all patients are reassessed for surgery. If the cancer has not spread to distant areas of the body, surgery will likely be offered.
Surgery for a Pancoast Tumor
Prior to surgery, the doctor carefully assesses and stages the cancer. During surgery, the doctor usually removes a portion of the chest wall and part of the lung. The survival rate associated with this procedure is typically 30% to 50% after five years.
People with Pancoast tumors that are directly invading the covering of the lung and chest wall should generally undergo surgery, if:
- The cancer has not spread to distant parts of the body.
- The patient's heart and lungs are healthy enough to allow surgery.
- There is no evidence of extensive enlargement of the lymph nodes.
The patient's outlook is then dependent on the status of the lymph nodes. Occasionally, people with severe pain who have tumors that can't be removed may be selectively considered for palliative surgery to reduce pain.
Preventing Pancoast Tumor
The most important preventive step is to avoid using tobacco products. Quitting tobacco also reduces the risk of lung cancer.
Taking precautions to reduce exposure to harmful substances in the environment (such as asbestos) can also reduce the risk of developing lung cancer.
Outlook for Pancoast Tumor
In the past, Pancoast tumors were considered inoperable and incurable because of their relative inaccessibility and extensive invasion of nearby tissues and structures. However, recent studies have shown that, in some people, the tumor completely stops growing and the pain is gone. In addition, survival rates have improved. In the early stage there is a 30%-50% survival rate at 5 years.
Studies demonstrate that radiation and chemotherapy -- before surgery -- in doses strong enough to shrink the tumor:
- Decrease the chance that the tumor will grow back
- Prevent tumor cells from growing elsewhere in the body
- Increase the chance of survival compared with radiation, chemotherapy, or surgery alone