1 of 11 / Overview
View All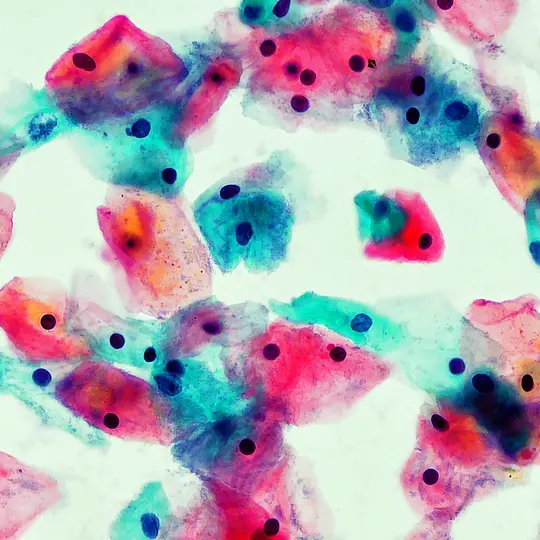
What Is Cancer?
Cancer starts when a cell is somehow altered so that it multiplies out of control.
Is There a Cure for Cancer?
There’s no cure for it, but there are treatments that may be able to cure some people of some cancers.
Cancer Incidence by Age
You’re more likely to get cancer as you get older. In fact, age is the biggest risk factor for the disease.
2 of 11 / Causes, Risks & Prevention
View All
Common Carcinogens
A carcinogen is something that can cause you to have cancer.
Smoking and Cancer
Smoking cigarettes causes about 3 out of every 10 cancer deaths in the U.S.
Alcohol and Cancer
Researchers found that drinking alcohol causes chemical and other physical changes in our bodies that make cancers more likely.
Viruses That Can Lead to Cancer
You might be surprised to learn that some viruses can lead to cancer.
3 of 11 / Symptoms & Types
View All
Early Signs of Cancer
Pay attention to your body. Play it smart when you notice anything that could be a serious health problem, like cancer.
Cancer Symptoms Women Ignore
It’s a good idea to get any new symptoms checked out by your doctor. Some changes could be signs of cancer.
Common Cancers and How to Spot Them
Most people know of someone in their family who has been diagnosed with cancer. So it’s helpful to know cancer warning signs.
Cancers That Metastasize to the Bones
Bones, lungs, and the liver are the most common places for cancer cells to spread, or "metastasize."
4 of 11 / Tests & Diagnosis
View All
Cancer Diagnosis
Some types of cancer may be detected by routine self-exam or other screening measures before the symptoms become serious.
Cancer Diagnosis Without Biopsy
You can find certain types of cancer without a biopsy. There are a few different ways to do this.
Lymph Node Biopsy
If your doctor says you should get a lymph node biopsy, it's because they need to check for signs of disease, such as cancer.
Bone Biopsy
A bone biopsy is a test that takes a sample of tissue or cells from your bone to check for cancer or other bone diseases.
5 of 11 / Your Cancer Care Team
View All
Cancer Specialists
Most cancers are complex to treat, so you may need to see several different cancer specialists during your treatment.
What Is Medical Oncology?
Medical oncology is a type of medicine that focuses on the diagnosis, treatment, and prevention of cancer.
What Is a Radiation Oncologist?
Radiation oncologists work with oncologists, surgeons, and other doctors to determine an appropriate course of treatment.
What Is Surgical Oncology?
Surgical oncology is a field of medicine that uses surgery to treat cancer. Its goal is to find tumors and remove them.
6 of 11 / Treatment & Side Effects
View AllCancer Treatment: What Are the Options?
You and your doctor will decide what treatment is best based on the type of cancer, where it is, and how far it has spread.
Cancer Surgery
If you have cancer, you may have surgery at some point. Sometimes, it can completely treat the disease.
Nuclear Medicine
Nuclear medicine can help diagnose and treat different conditions, including some forms of cancer.
New Ideas in Cancer Treatment
A lot has happened in recent years to transform how cancer is, and will be, treated.
7 of 11 / Treatment Support
View AllNatural Help for Treatment Side Effects
Cancer treatments like chemotherapy and radiation may save your life. But they can also cause unwelcome side effects.
Exercise During Cancer Treatment
Recent research suggests that exercise is not only safe, but helpful during your cancer treatment.
What Medicines Help Treat Cancer Pain?
When cancer causes you physical pain, there are many medicines that can help manage it so you feel better.
Ways Dogs Ease Cancer Treatment
Therapy dogs can bring comfort to people being treated for cancer, and they may help them get better, too.
8 of 11 / Living With
View AllTips for Living a Longer, Fuller Life With Cancer
There’s plenty you can do every day to not only survive cancer, but to feel better and live as well as you can.
Intimacy After Cancer
After cancer treatment, your sex life may be a little different than it used to be.
Cancer and Diet
What you eat is really important when you have cancer. Your body needs enough calories and nutrients to stay strong.
Fruits to Eat When You Have Cancer
While going through cancer treatment or trying to keep cancer from coming back, some fruits may be better than others.
9 of 11 / Remission & Recurrence
View All10 of 11 / Support & Resources
View AllHow to Tell Your Family and Friends You Have Cancer
If you’ve been diagnosed with cancer, you might be wondering when and how to break the news to your friends and family.
Hiring a Cancer Caregiver
Zero in on any gaps in care. Talk with your health care team to figure out where you might need extra support.
Cancer Caregiver's Checklist
While caring for someone with cancer, you want them know you're there to help. Use this checklist to make daily care easier.
How Health Care Reform Affects Your Cancer Care
If you have cancer, the Affordable Care Act gives you protection against losing insurance coverage.
11 of 11 / Appointment Prep
View AllQuestions for Your Doctor About Chronic Lymphocytic Leukemia
Whether you're newly diagnosed with CLL or already in treatment, learn how to make the most of your doctor appointment.
Questions for Your Doctor About Polycythemia Vera
Whether you're newly diagnosed with this blood cancer or already in treatment, learn how to make the most of your doctor appointment.
Questions for Your Doctor About Myelodysplastic Syndromes
Whether you're newly diagnosed with MDS or already in treatment, learn how to make the most of your doctor appointment.
Questions for Your Doctor About Myelofibrosis
Whether you're newly diagnosed with myelofibrosis or already in treatment, learn how to make the most of your doctor appointment.
Suggested Reads about Cancer
Expert Q&A: How to Tell Your Kids About Your Cancer
After Princess Kate’s cancer diagnosis announcement, read how experts advise telling kids that a parent has cancer.
Q&A: Precision Medicine for Black Americans With Cancer
Clayton Yates, PhD, at Johns Hopkins searches for new biomarkers and treatments for African Americans with prostate cancer, breast cancer, and more.
Cancer-Preventing Diet: Lowering Your Risk for Disease
Nutritionists are sounding the alarm on just how much your dietary consumption can affect your risk – or lack thereof – for cancer. A whopping 25% of the 18 million cancer cases in the U..S could be prevented by improving your nutrition.
Study: Alcohol, White Bread Linked to Colorectal Cancer Risk
New research shows that consuming high amounts of white bread and alcohol is associated with a greater risk of developing colorectal cancer.
8 million+ Physician Ratings & Reviews
Find Doctors and Dentists Near You
You can also search by physician, practice, or hospital name