What Is Oral Cancer?
Oral cancer most often appears as a growth or sore in your mouth that doesn't go away. It's a kind of head and neck cancer. You may hear it called mouth cancer or oral cavity cancer. If it's in the back of your mouth or upper throat, that's oropharyngeal cancer.
More than 50,000 people in the U.S. get oral cancer each year. It can be life-threatening if not diagnosed and treated early.
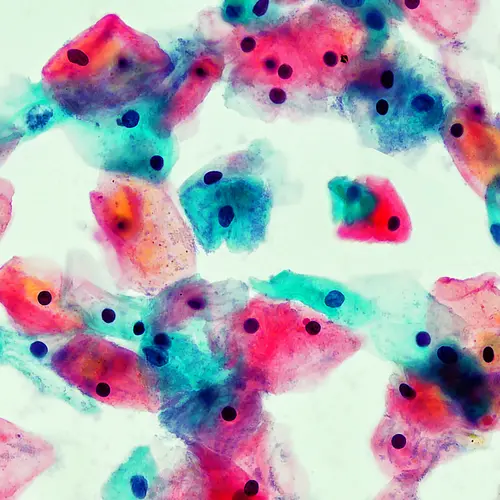
Oral cancer manifestations
Most oral cancers begin in what are called squamous cells in the layer of tissue that lines your mouth and throat. Something changes the DNA inside the cells, causing them to grow out of control into a tumor.
Oral cancer can appear in many different spots, including:
When it's caught early, oral cancer is much easier to treat, so it's important to learn how to spot suspicious changes in your mouth.
Oral Cancer Symptoms
The most common symptoms of oral cancer include:
- A sore on your lip or in your mouth that doesn't heal
- A lump or thick patch inside your mouth or throat
- White, red, or speckled (white and red) patches in your mouth or throat
- Unexplained bleeding in your mouth
- Unexplained pain or numbness in your mouth or throat
- Chronic sore throat, or a feeling that something is caught in the back of your throat
- Trouble chewing or swallowing, speaking, or moving your jaw or tongue
- Hoarseness or change in your voice
- Ear pain
- Swelling, pain, or stiffness in your jaw
- A lump in your neck
- A change in the way your teeth fit together, or loose teeth (if you wear dentures, they might be uncomfortable or hard to put in)
- Dramatic weight loss
- Chronic bad breath
If you notice any of these changes, and they last more than 2 weeks, let your dentist or doctor know.
What does oral cancer look like?
On your lip, oral cancer often looks like a cold sore. You may notice a white or red spot if you have light-colored skin. The sore may look dark brown or gray on dark skin. It may be bloody or crusty.
Inside your mouth, oral cancer may look like a white or red spot on your gums, tongue, inside of your lips or cheeks, roof of your mouth, or under your tongue. It resembles a canker sore but doesn't hurt as much.
Oral cancer may also appear as a lump on your gum or other parts of your mouth.
Oral Cancer Risk Factors
According to the American Cancer Society, people assigned male at birth face twice the risk of developing oral cancer as people assigned female at birth. It's estimated that over 54,000 people in the U.S. will have received a diagnosis of oral cancer in 2023.
Risk factors for the development of oral cancer include:
Smoking. The vast majority of oral cancers can be traced to cigarette, cigar, or pipe smoking. E-cigarettes may not be any safer. Vaping hasn't been studied as much as smoking, but some research shows it can cause the same kind of cell damage that leads to oral cancer.
Smokeless tobacco use. Using dip, snuff, or chewing tobacco products makes you much more likely to develop cancers of the cheek, gums, and lining of the lips.
Drinking too much alcohol. Oral cancers are about five times more common in drinkers than in nondrinkers. Using alcohol and tobacco together increases your chances even more.
A family history of cancer.
Excessive sun exposure, especially at a young age. Ultraviolet radiation from the sun can cause lip cancers.
Human papillomavirus (HPV). A specific type of HPV is linked to more than two-thirds of oropharyngeal cancers, which affect areas such as the back of the tongue, throat, and tonsils. It's becoming more common in younger people and in people who have multiple sex partners.
Age. Oral cancers can take years to grow. Most people find they have it after age 55. But cancers caused by HPV are showing up in younger people.
Gender. People assigned male at birth are more than twice as likely as people assigned female at birth to get oral cancer. It could be because of gender differences in how much people drink and smoke.
Poor diet. Studies show a link between oral cancer and not eating enough vegetables and fruits.
Weakened immune system. When your body's natural defenses against infection are lowered because of an illness (such as an HIV infection) or medications (such as chemotherapy), you're more vulnerable to HPV.
Oral Cancer Survival Rate
How well oral cancer responds to treatment depends in part on how advanced it is when you find it. For patients with an early diagnosis of oral cavity and throat cancers, the overall 5-year survival rate is 86%. If the cancer has spread to nearby tissues, organs, or lymph nodes, the 5-year survival rate drops to 69%.
Oral Cancer Diagnosis
As part of your routine dental exam, your dentist will screen you for oral cancer. Your dentist knows what a healthy mouth should look like and probably has the best chance of spotting any cancer. Experts recommend getting checked every year starting at age 18, and sooner if you start smoking or having sex.
More specifically, your dentist will feel for any lumps or irregular tissue changes in your neck, head, face, and oral cavity. In your mouth, your dentist will look for sores or discolored tissue.
If they find something suspicious, the next step is to take a sample of tissue to check under a microscope. That's called a biopsy. They may refer you to a specialist or do the test themselves.
There are different types of biopsies, and your doctor can decide which one is best.
Oral brush biopsy. Cells are collected by gently scraping the area with a special brush.
Incisional biopsy. The doctor cuts out a small piece of tissue. Depending on how the suspicious spot looks to them, they may remove it entirely as well as some surrounding tissue.
Fine needle aspiration. This procedure is used to check a lump in your neck or lymph node. The doctor inserts a thin, hollow needle and draws out a sample of cells with a special kind of syringe.
Staging Oral Cancer
If a biopsy shows that you have oral cancer, you'll get other tests to find out whether you have cancer anywhere else. Then the tumor will be assigned a stage based on how big it is and how far it has spread. Not everyone needs every test, but they may include:
Endoscopy. Your doctor looks down your throat with a special camera attached to a flexible tube. They can take samples of any spots that look suspicious.
Imaging tests, including MRI and CT scans. MRI and CT scans are among the tests that help your doctor pinpoint the size and location of the tumor. They can also show whether cancer has spread to your lymph nodes or other parts of your body.
HPV test. If you have cancer in your throat or the back of your tongue, tumor cells will likely be tested for HPV. The presence or absence of this virus plays a role in staging.
Cancer staging helps your doctor decide the best course of treatment for you and give you an idea of how well you'll recover.
For oral and oropharyngeal cancer, staging begins by describing the tumor with a system called TNM, which stands for tumor, node, and metastasis. It's a series of letters and numbers that's a kind of code for the size of the tumor, whether lymph nodes are involved, and whether the cancer has spread (metastasized) to other parts of your body.
That code gets translated into a number from zero to four that tells you how serious the cancer is. The stage groups are different depending on whether HPV is involved.
Oral or oropharyngeal cancer without HPV
- Stage 0 (Tis, N0, M0):The tumor is only in the surface layer of cells (carcinoma in situ) and hasn't spread to your lymph nodes or the rest of your body.
- Stage I (T1, N0, M0): The tumor is in the deeper layer of cells, but it's 2 cm or smaller and hasn't spread anywhere else.
- Stage II (T2, N0, M0): The tumor ranges from 2 to 4 cm in size but hasn't spread.
- Stage III (T3, N0, M0 or T1 to T3, N1, M0): Either the tumor is larger than 4 cm, or it's 3 cm or smaller, and you have cancer in one lymph node, or the cancer has spread to your epiglottis.
- Stage IVA (T4a, N0 or N1, M0 or T1 to T4a, N2, M0): The cancer has spread to other parts of your mouth or face and may involve more than one lymph node.
- Stage IVB (any T, N3, M0 or T4b, any N, M0):The cancer may have spread to the tissue surrounding a lymph node or to more parts of your head and neck.
- Stage IVC (any T, any N, M1): The cancer has spread to other parts of your body.
Oropharyngeal cancer with HPV
- Stage I (T0 to T2, N0 or N1, M0): The tumor is 4 cm or smaller and may have spread to a few lymph nodes, but nowhere else in your body.
- Stage II (T0 to T2, N2, M0 or T3 or T4, N0 to N2, M0): The tumor may be bigger than 4 cm, has spread to more lymph nodes, or has spread to your epiglottis.
- Stage III (any T, N3, M0 or T4, any N, M0): The tumor is bigger, or the cancer has spread to other parts of your mouth or face.
- Stage IV (any T, any N, M1): The cancer has spread to other parts of your body.
Oral and oropharyngeal tumors may also be assigned a grade from one to four. This tells how much tumor cells look like healthy cells. The lower the grade, the less likely the tumor will spread.
Oral Cancer Treatment
Oral cancer is treated the same way many other cancers are treated, using methods such as surgery to remove the cancerous growth, radiation therapy and drug treatments to kill cancer cells, or a combination of these.
It's recommended that you see your dentist at least a month before you start treatment to take care of any tooth or gum problems that could make your recovery harder. It will also give you time to heal from the dental work.
Surgery
This is usually the first option for oral cavity cancers.
A surgeon will remove the tumor and any surrounding tissue containing cancer cells. Depending on where it's located, they may do this through your mouth or a cut in your neck. Your doctor may also want to remove lymph nodes to make sure the cancer doesn't spread.
You may have to have large sections of your tongue, jawbone, or the roof of your mouth removed. If that's the case, you may also get reconstructive surgery to help you eat and speak.
After surgery, you may have radiation or drug therapy to destroy any remaining cancer cells.
Radiation therapy
This could be a follow-up treatment to surgery, or your main treatment if surgery isn't an option. It's also the main treatment for throat cancer.
High-powered X-rays are focused on the spot where the cancer is located for a few minutes at a time. For oral cancer, it's common to have the treatment every day for several weeks. Radiation is also sometimes combined with chemotherapy, especially with throat cancer.
Medication therapy
Different kinds of cancer-fighting drugs may be used as a follow-up to surgery, or for oral or oropharyngeal cancer that has spread or comes back after treatment.
Chemotherapy. This involves drugs that kill cancer cells as well as other cells. You may get chemotherapy to shrink a tumor before surgery, or after surgery to kill any remaining cancer cells. It could be your main treatment if surgery isn't an option.
Immunotherapy. These drugs help your body's natural defense system identify and attack cancer cells. This type of treatment is approved for oral cancer that doesn't respond to chemotherapy.
Targeted therapy. This treatment uses drugs designed to work only against cancer cells. Your doctor will test your tumor cells for certain genetic information to decide which drug would work best. You may get this treatment in combination with radiation or chemotherapy.
Oral cancer recovery
Treatment for oral cancer can change your appearance and affect your ability to eat and speak. While you're recovering, you'll need help managing pain and other side effects, plus nutritional and emotional support. You may hear this called palliative care.
You'll have follow-up visits with your doctor and tests every few months for the first 3 years to check your recovery and make sure the cancer hasn't come back.
Treatment side effects. Oral cancer treatments can damage healthy tissue and cause new health problems. Ask your doctor what side effects you can expect. Not everyone has all of them, but you may have:
- Pain and inflammation in your mouth
- Trouble chewing, swallowing, or opening your mouth
- Swelling that makes it hard to breathe
- Speech changes
- Taste changes
- Dry mouth, thickened saliva, mouth sores, and tooth decay from removal of or damage to salivary glands
- Thyroid problems
- Ear numbness or hearing problems
- Redness or skin irritation in areas being treated with radiation
- Digestive issues including, nausea, vomiting, diarrhea, and constipation
- Fatigue
- Hair loss
- Weakened immune system that increases your risk of infection
Some side effects go away when you're finished with treatment, but others can last much longer or be permanent. Tell your doctor about any problems you're having so they can help you manage them.
Nutritional support. Oral cancer and treatments for it can make eating a challenge. On top of mouth pain and trouble chewing and swallowing, food may taste different, and you may just not feel like eating. That can lead to weight loss, weakness, and malnutrition. You may need a feeding tube for some time. You can also work with a nutritionist to find the best way to get enough calories and other nutrients while you recover.
Speech therapy. A speech therapist can help you manage both speech problems and trouble swallowing. If treatment has caused hearing loss, an audiologist can help you find a solution.
Emotional support. It's common to have anxiety and depression while you're going through cancer treatment. Connecting with others through a support group, either in person or online, can be helpful. Your doctor can also refer you to a social worker, counselor, or therapist who can help you deal with the process.
Oral Cancer Prevention
Scientists think that oral cancer starts when the DNA in the cells inside your mouth gets damaged. But some things, including your health habits, can make you more likely to get it. To lower your risk of oral cancer:
- Get vaccinated against HPV.
- Don't smoke or use any tobacco products. If you drink alcohol, do so only in moderation.
- Eat a well-balanced diet. Not getting a lot of fruits and vegetables has been linked to an increased risk of oral cancer.
- Limit your exposure to the sun. Repeated exposure increases your risk of lip cancer. When in the sun, use UV-A/B-blocking sunscreen on your skin, and don't forget your lips.
Regular screening can't prevent oral cancer but can catch the cancer early when it's easier to treat. Regular screening may include:
Conducting a self-exam at least once a month. Your doctor may recommend this if you smoke or drink heavily. Here's what you can do:
- Using a bright light and a mirror, look at and feel your lips and front of your gums.
- Tilt your head back and look at and feel the roof of your mouth.
- Pull your cheeks out to see the inside of your mouth, the lining of your cheeks, and your back gums.
- Pull out your tongue and look at all surfaces; examine the floor of your mouth.
- Look at the back of your throat.
- Feel for lumps or enlarged lymph nodes on both sides of your neck and under your lower jaw.
Make an appointment to see your dentist as soon as possible if you notice any changes in the appearance of your mouth, such as white spots or sores.
Getting regular dental checkups. Even if you do self-checks, you may not catch every dangerous spot. You should have an oral cancer screening at least once a year when you visit the dentist for a cleaning.
Takeaways
Oral cancer often appears as a white patch or sore in your mouth. While anyone can get it, it's mainly linked to smoking, heavy drinking, and infection with the human papillomavirus (HPV). Treatments include surgery, radiation, and drug treatments such as chemotherapy. It's easier to treat if it's caught early, so get screened by your dentist at least every year.
Oral Cancer FAQs
Can mouth cancer be cured?
Yes, especially if it's found at an early stage when it's still small and hasn't spread.
What is the life expectancy of a person with mouth cancer?
Survival rates are very different depending on where the cancer is and how advanced it is when you're diagnosed. If it's caught early, 86% of people with oral cavity or throat cancers will live at least 5 years. If the cancer has spread to nearby tissues, organs, or lymph nodes, the 5-year survival rate drops to 69%.