- Overview & Types
- Symptoms & Diagnosis
- Treatment
- Living With
- Related Conditions
- Type 2 Diabetes
- Type 1 Diabetes
- Gestational Diabetes
- Appointment Prep
- View Full Guide
Your Type 1 Diabetes Care Plan


Be Proactive
Juggling food, exercise, insulin, and testing can seem like a circus act. But it doesn't have to be that way. A written care plan can help you keep all the balls in the air. With your diabetes care team, craft one that accounts for your changing needs. Together, you can keep blood sugar in its "sweet" spot.

It Starts With Insulin
You have to take insulin to get glucose out of your blood and into your cells for energy. Some types work slowly and last most of the day. Others work fast but don't last long. You may need several types of insulin to control your blood sugar around the clock -- and avoid problems like kidney, nerve, and eye damage.

Shots or Pump?
You can inject yourself with insulin in a syringe or an injection pen. You'll probably need shots several times a day.
Or you can use a pump. It sits in your pocket or on a belt. The pump is connected to your body with a tube and a needle under the skin. It releases insulin slowly and continuously. You can also program the pump to deliver more insulin when you need it.

Know Your Numbers
Glucose testing tells you if your blood sugar is on target. You'll probably need to check it four to eight times a day. Usually, you do it before meals, at bedtime, and before and after exercise.
Your plan should tell you what to do if your sugar isn't where it needs to be: A little high, drink water or take a brisk walk; too low, drink a half-cup of fruit juice.

Check In With Your Team
Visit your medical team at least four times a year. You might go more often when you have trouble controlling your blood sugar or if you have other problems.
Sometimes, you'll get blood tests. For example, the A1c tracks your "average" blood sugar over the past few months. Your doctor may change your treatment (and your plan), based on the results. You may also need to see specialists.

Eat Right
Generally, your diet should favor non-starchy veggies like greens, carrots, and broccoli. You'll need to limit carbohydrates like potatoes and pasta, and sweets like cake. Get your protein from lean, low-fat sources like chicken, fish, and beans and legumes. Your care team can help you come up with a food plan that also considers what you like, any cultural or religious traditions, and other concerns like allergies.
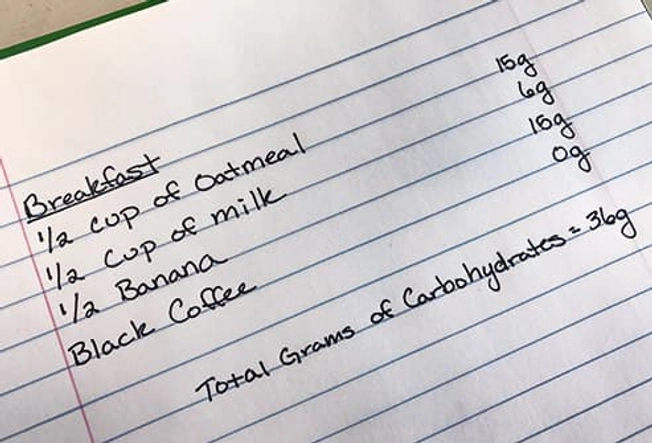
Do the Math
Since carbs raise your blood sugar more than other foods, counting the carbs in what you eat can help keep your blood sugar steady. Your plan should tell you how many to have in each meal or snack. Often, that's 45-60 grams, but how much you need will depend on things like how active you are.

Timing Matters, Too
When you eat is as important as what you eat. Many people with type 1 diabetes need to eat around the same times each day. If you take insulin with meals (rapid or short-acting) or use a pump, you may have a bit more flexibility. Don't skip meals. That can throw off the delicate balance between glucose and insulin. Your blood sugar can dip dangerously low (hypoglycemia).

Save Room for Dessert (Sometimes)
Cakes, cookies, ice cream, and other sweets are often part of celebrations. You can share in the merriment, but you'll need to think ahead. On special occasions, it's OK to "spend" your carbs on a treat instead. You could skip the rolls or mashed potatoes during dinner so you can have a small slice of Grandma's pie. But don't make it a regular swap.

Get Physical
Exercise helps move sugar into your cells without using insulin, so it's an important way to help manage your diabetes. Since activity affects your blood glucose, test before and after (and during, if you're at it for a while) to avoid hypoglycemia.
Sometimes, a workout can spike your sugar. Usually, this happens when intense or long exercise raises hormones that boost glucose.

Offset Lows
When your blood sugar is under the target number for exercise in your plan, have about 15 grams of carbs -- maybe a few ounces of sports drink or fruit juice -- then wait 15 minutes and test again. Eat a high-carb snack if your glucose is low afterward, too.
Hold for Highs
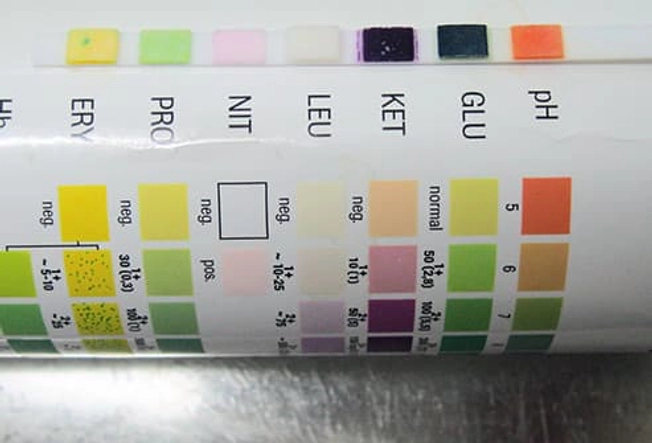
If you test high before exercise (250 mg/dL or more), check your urine for ketones. It's OK to work out if you don't have them, but don't push yourself hard. If you do have ketones, stop. Your body is using fat instead of glucose for fuel, and you could get ketoacidosis -- a medical emergency. Check with your team about how to deal with it.

Set Up for Sick Days
The hormones your body makes to fight illness also raise your glucose and make insulin less effective, which can lead to ketoacidosis. Throwing up or diarrhea may make managing blood sugar a real challenge. And you're not going to want to think about it when you aren't feeling well. Having a "sick day roadmap" ready ahead of time will help get you through.

Keep Testing
You'll need to check your blood more often -- about every 3 hours -- so you can make adjustments to keep your glucose on target. For high sugar, your plan may call for more insulin and follow-up urine tests for ketones. Keep a record of all these results. They could help your doctor.

Try to Eat Regularly
Stick to your usual diet plan, if you can. If not, pick foods that are easier on your tummy, like crackers, applesauce, and soup. Can't handle solid food? Suck on frozen juice bars for carbs. Make sure you're drinking enough, too. You can get dehydrated when you have a fever, the runs, or you're throwing up. Water or another no-calorie drink can help flush-out glucose and maybe ketones, too.

When to Call for Help
Have ways to get in touch with your care team and emergency contacts, including after hours. Pick up the phone if:
- You can't get your blood sugar below 240.
- You have more than a few ketones.
- You haven't been able to keep anything down or in for more than 6 hours.
- You're confused, aren't breathing well, or have fruity breath -- which could be ketoacidosis.

Going Mobile
If you need to take short breaks to test your blood sugar or inject insulin at work, you're protected by law. Stash a diabetes care kit at your job, stocked with lancets, test strips, a monitor, batteries, unopened insulin and syringes, glucose tablets and juice boxes, and a glucagon shot in case you pass out from hypoglycemia. When you're traveling, make sure the care kit goes with you, too.

Enlist a Buddy
You need someone to have your back in case there's a time when you can't help yourself. Ask a trusted friend or co-worker to learn the signs of a diabetic emergency (very high or very low blood sugars), where to find your care kit, how to use the glucagon kit, and when to call 911.