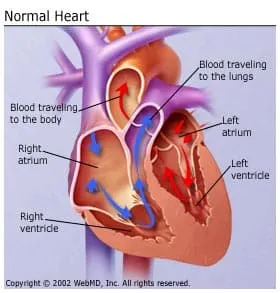
In the normal heart, the heart's lower chambers (ventricles) pump in sync with the heart's upper chambers (atria).
When a person has heart failure, often the right and left ventricles do not pump synchronously. And when the heart's contractions become out of sync, the left ventricle may not be able to pump enough blood to the body.
This eventually leads to an increase in heart failure symptoms, such as shortness of breath, dry cough, swelling in the ankles or legs, weight gain, increased urination, fatigue, or rapid or irregular heartbeat.
Cardiac resynchronization therapy (CRT), also called biventricular pacing, uses a special kind of pacemaker, called a biventricular pacemaker, designed to help the ventricles contract more normally.
It keeps the right and left ventricles pumping in sync by sending small electrical impulses through the leads.
This therapy has been shown to improve the symptoms of heart failure and overall quality of life in certain patients with significant symptoms that aren't controlled with medication.
What Is a Biventricular Pacemaker?
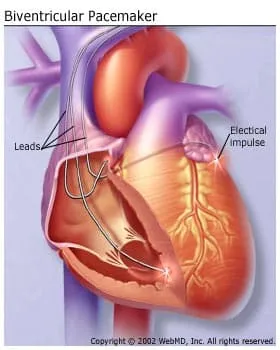
Leads are tiny wires implanted through a vein into the right ventricle and into the coronary sinus vein to pace or regulate the left ventricle. Usually (but not always), a lead is also implanted into the right atrium. This helps the heart beat in a more balanced way.
Traditional pacemakers are used to treat slow heart rhythms. Pacemakers regulate the right atrium and right ventricle to maintain a good heart rate and keep the atrium and ventricle working together. This is called AV synchrony. Biventricular pacemakers add a third lead to help the left ventricle have a more efficient contraction.
Who Is a Candidate for a Biventricular Pacemaker?
Biventricular pacemakers improve the symptoms of heart failure in about 50% of people that have been treated with medications but still have significant heart failure symptoms. Therefore, to be eligible for the biventricular pacemaker, heart failure patients must:
- Have heart failure symptoms
- Be taking medications to treat heart failure
- Have the type of heart rhythm problems mentioned above (Your doctor can usually determine this using ECG testing.)
In addition, the heart failure patient may or may not need this type of pacemaker to treat slow heart rhythms and may or may not need an internal defibrillator (implantable cardioverter defibrillator, or ICD), which is designed to treat people at risk for sudden cardiac death or cardiac arrests.
My Doctor Recommends Combination ICD and Pacemaker Therapy. Why?
People with heart failure who have poor ejection fractions (measurement that shows how well the heart pumps with each beat) are at risk for fast irregular heart rhythms -- some of which can be life-threatening -- called arrhythmias. Currently, doctors use an ICD to prevent these dangerous rhythms. The device works by detecting such a rhythm and shocking the heart back to normal.
These devices can combine biventricular pacing with anti-tachycardia (fast heart rate) pacing and internal defibrillators (ICDs) to deliver treatment as needed. Current studies are showing that resynchronization may even lessen the amount of arrhythmia that occurs, decreasing the times the ICD needs to shock the heart. These devices are helping heart failure patients live longer and improving their quality of life.
How Do I Prepare for the Biventricular Pacemaker Implant?
Ask your doctor what medications you are allowed to take before your pacemaker is implanted. Your doctor may ask you to stop certain drugs several days before your procedure. If you have diabetes, ask your doctor how you should adjust your diabetic medications.
Do not eat or drink anything after midnight the night before the procedure. If you must take medications, drink only small sips of water to help you swallow your pills.
When you come to the hospital, wear comfortable clothes. You will change into a hospital gown for the procedure. Leave all jewelry and valuables at home.
What Happens During the Pacemaker Implantation?
Pacemakers can be implanted two ways:
Inside the Heart (Endocardial, Transvenous approach): This is the most common technique used. A lead is placed into a vein (usually under your collarbone), and then guided to your heart. The tip of the lead attaches to your heart muscle. The other end of the lead is attached to the pulse generator, which is placed under the skin in your upper chest. This technique is done under local anesthesia (you will not be asleep).
Outside the Heart (Epicardial approach): Your chest will be opened and the lead tip is attached to the outside of the heart. The other end of the lead is attached to the pulse generator, which is placed under the skin in your abdomen. This technique is done under general anesthesia (you will be asleep) by a surgeon. This is typically performed in conjunction with open heart surgery being performed for another reason.
Your doctor will decide which approach is best for you, although almost all patients receive the transvenous approach.
A Closer Look at What Happens During the Endocardial Approach
- Your procedure will take place in the electrophysiology (EP) lab, catheterization lab, or operating room. You will lie on a bed and the nurse will start an IV (intravenous) line to deliver medications and fluids during the procedure. An antibiotic will be given through your IV at the beginning of the procedure to help prevent infection. You will receive a medication through your IV to make you drowsy. The medication will not put you to sleep. If you are uncomfortable or need anything during the procedure, please let the nurse know.
- The nurse will connect you to several monitors. The monitors allow the doctor and nurse to monitor your condition at all times during the procedure.
- Because it is very important to keep the area of insertion sterile to prevent infection, your chest will be shaved (if necessary) and cleansed with a special soap. Sterile drapes will be used to cover you from your neck to your feet. A soft strap will be placed across your waist and arms to prevent your hands from coming in contact with the sterile field.
- The doctor will numb your skin by injecting a local numbing medication. You will feel a pinching or burning feeling at first. Then the area will become numb. Once this occurs, an incision will be made to insert the pacemaker and leads. You may feel a pulling as the doctor makes a pocket in the tissue under your skin for the pacemaker. You should not feel pain. If you do, tell your nurse.
- After the pocket is made, the doctor will insert the leads into a vein and guide them into position using a fluoroscopy machine.
- After the leads are in place, the doctor tests the leads to make sure lead placement is correct, the leads are sensing and pacing appropriately and the right and left ventricles are synchronized. This is called "pacing" and involves delivering small amounts of energy through the leads into the heart muscle. This causes the heart to contract. When your heart rate increases, you may feel your heart is racing or beating faster. It is very important to tell your doctor or nurse any symptoms you feel. Any pain should be reported immediately.
- After the leads are tested, the doctor will connect them to your pacemaker. Your doctor will determine the rate of your pacemaker and other settings. The final pacemaker settings are done after the implant using a special device called a "programmer."
- The pacemaker implant procedure lasts one to two hours. A biventricular pacemaker may take longer.
What Happens After The Pacemaker Is Implanted?
Hospital stay: After the pacemaker implant, you will be admitted to the hospital overnight. The nurses will monitor your heart rate and rhythm. You will also have a monitor (a small recorder that is attached to your chest by small electrode patches). It will record your heart rhythm while you are in the hospital. This is another way to check proper pacemaker function. The morning after your implant, you will have a chest X-ray to check your lungs and the position of your pacemaker and leads. Your pacemaker will be checked to make sure it's working properly. The results of the test will be reported to your doctor.
Final pacemaker check: For your final pacemaker check, you will sit in a reclining chair. A small machine known as a programmer is used to check your pacemaker. It has a wand that is placed directly over the device. This machine allows the technician to read your pacemaker settings and make changes during testing. With these changes, the function of the pacemaker and leads can be evaluated. You may feel your heart beating faster or slower. This is normal; however, report all symptoms to the technician. Results of the pacemaker check are discussed with your doctor who will then determine your pacemaker settings.
After your pacemaker check, an echocardiogram may be done. The technician nurse will be there during your echo and will check your pacemaker settings. The echocardiogram will be repeated with each setting to evaluate heart function. The pacemaker will keep the settings that were associated with your best heart function.
When Will I Be Able to Go Home After a Pacemaker Implant?
Usually, you will be able to go home the day after your pacemaker is implanted. Your doctor will discuss the results of the procedure and answer any questions you may have. A doctor or nurse will go over specific instructions for your care at home. Please ask a responsible adult to drive you home, as the medications you received may cause drowsiness, making it unsafe for you to drive or operate heavy machinery.
How Do I Care for My Wound?
Keep the area where the pacemaker was inserted clean and dry. After about five days, you may take a shower. Look at your wound daily to make sure it is healing. Call your doctor if you notice:
- Increased drainage or bleeding from the insertion site
- Increased opening of the incision
- Redness around the incision site
- Warmth along the incision
- Increased body temperature (fever or chills)
When Can I Do Normal Activities After a Pacemaker Implantation?
After your pacemaker is implanted, you may move your arm; you don't have to restrict its motion during normal daily activities. Avoid extreme pulling or lifting motions (such as placing your arm over your head without bending at the elbow). Activities such as golf, tennis, and swimming should be avoided for six weeks from when the pacemaker was implanted. Microwave ovens, electric blankets, and heating pads may be used. Cellular phones should be used on the side opposite your pacemaker. Ask your doctor or nurse for more specific information regarding what types of equipment may interfere with your pacemaker.
Pacemaker Identification: You will receive a temporary ID card that tells you what type of pacemaker and leads you have, the date of implant and the doctor who implanted it. In about three months following implantation, you will receive a permanent card from the company. It is important that you CARRY THIS CARD AT ALL TIMES in case you need medical attention at another hospital.
How Often Do I Need to Get the Pacemaker Checked?
Your medical team will arrange for a complete pacemaker check after your pacemaker is implanted. This check is very important because adjustments will be made that can prolong the life of your pacemaker. After that, your pacemaker should be checked every six months using a telephone transmitter to evaluate battery function. The nurse will explain how to check your pacemaker using the telephone transmitter. When the battery gets low, you will need to replace your pacemaker.
A follow-up pacemaker check is scheduled every three to six months. This check differs from the telephone check because the leads are also tested. Leads cannot be checked thoroughly over the telephone.
Here is an outline of a typical pacemaker follow-up schedule:
- Check before you are discharged from the hospital, the day after implant
- Telephone call two weeks after implantation to make sure the wound is healing and to ensure the transmitter is working
- Six-week check
- Telephone checks every three to six months starting three months after your six-week check
- Pacemaker analysis every three to six months (in between telephone checks)
How Long Will My Pacemaker Last?
Pacemakers usually last 6 to 10 years. Biventricular pacemakers that are combined with an ICD do not tend to last as long.
How Will I Know if my Pacemaker Needs to Be Changed?
After getting a pacemaker, you will need to follow-up with the doctor and nurses in a pacemaker clinic and through phone check-ups. This will allow them to monitor your pacemaker's function and anticipate when it will need to be changed. In addition, the pacemaker may be programmed to beep when the battery is low. Your doctor will demonstrate this beep for you.
Resynchronization therapy is only one part of a comprehensive heart failure management program. Device and/or surgical therapy, when combined with taking medications, following a low-sodium diet, making lifestyle changes, and following up with a heart failure specialist, will help you decrease symptoms and live a longer, more active life. Your doctor will help determine what treatment options are best for you.
