This serious condition makes the pressure inside your eye (your doctor may call it intraocular pressure, or IOP) go up suddenly. It can rise within a matter of hours. It happens when fluid in your eye can’t drain the way it should. It isn’t as common as other types of glaucoma, which cause pressure buildup much more slowly over time.Acute angle-closure glaucoma is caused by a rapid or sudden increase in pressure inside the eye, called intraocular pressure (IOP).
Causes
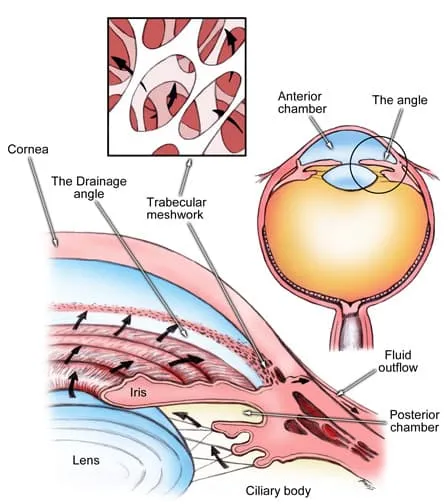
Fluid drains out of your eye through a system of canals. These canals live in a mesh of tissue between your iris (the colored part of your eye) and your cornea (the clear outer layer).
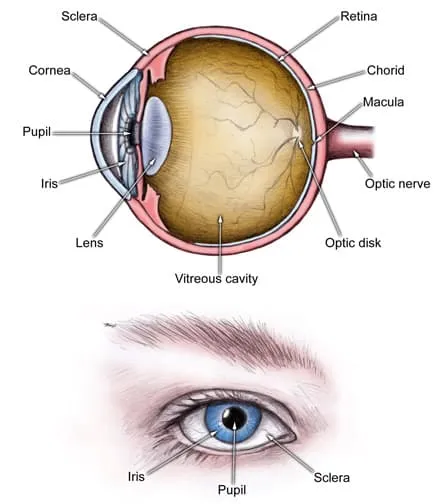
When your iris and cornea move closer together, it “closes the angle” between them. When this happens suddenly, it’s called an acute attack and is very painful.
Acute angle closure glaucoma completely blocks your canals. It stops fluid from flowing through them, kind of like a piece of paper sliding over a sink drain. The pressure that builds up can damage your optic nerve. If you don’t treat the problem quickly enough, you could lose your sight completely.
You might have an attack of angle closure glaucoma if you have narrow drainage systems and your eyes dilate (your pupil gets bigger) too much or too quickly. This can normally happen when you:
- Go into a dark room
- Get drops that dilate your eyes
- Are excited or stressed
- Take certain drugs like antidepressants, cold medications, or antihistamines
Some health conditions can also cause angle closure glaucoma:
- Cataracts
- Ectopic lens (when your lens moves from where it should be)
- Diabetic retinopathy
- Ocular ischemia (narrowed blood vessels to the eye)
- Uveitis (eye inflammation)
- Tumors
Women are 2 to 4 times more likely to get it than men. You’re also more likely to have it if you’re:
- Asian or Inuit
- Farsighted
- Between 55 and 65
Or if you:
- Have a family history of it
- Use medications that dilate your pupils
- Use other medications that cause your iris and cornea to come together, like sulfonamides, topiramate, or phenothiazines
If you have acute angle closure glaucoma in one eye, you’re also more likely to get it in the other.
Symptoms
They come on quickly. You won’t be able to ignore them. They include:
- Eye pain
- Severe headache
- Nausea or vomiting
- Very blurry or hazy vision
- Seeing rainbows or halos around lights
- Redness in the white part of the affected eye
- Pupils of different sizes
- Sudden loss of sight
When your doctor examines you, they may also notice that your pupils no longer get smaller or bigger when they shine light on them.
Diagnosis
If you think you have acute angle closure glaucoma, you’ll need to see an ophthalmologist right away -- it’s an emergency. They’ll examine you and ask about your symptoms. They may do one or more tests to find out more about what’s going on inside your eye:
- Gonioscopy: The doctor uses a lens with a simple microscope called a slit lamp to look into your eye. A beam of light checks the angle between your iris and cornea and see how well fluid drains.
- Tonometry: This test uses a tool to measure the pressure inside your eye.
- Ophthalmoscopy: Your doctor checks for damage to your optic nerve with a small lighted device.
Treatment
The first thing your doctor will do to treat your acute angle closure attack is try to get rid of some of the pressure in your eye. They might use:
- Drops that narrow your pupil
- Medication to lowers the amount of fluid your eye makes
Once your IOP has dropped a little, your doctor may use a laser to:
- Make a small hole in your iris. This is called a laser iridotomy, and it helps the fluid start flowing again inside your eye. It’s an outpatient treatment, and takes a few minutes.
- Pull the edges of your iris away from your drainage canals. This called laser iridoplasty or gonioplasty.
If you have cataracts, your doctor may consider surgery to replace the lens in your eye. This type of surgery can be harder to do when you’re having an acute attack.
Even if your acute angle closure glaucoma is in only one eye, your doctor will probably treat both eyes, just to be safe. You may need further surgery if this does not allow a passage for enough drainage of fluid.
Prevention
The best way to prevent an acute angle closure glaucoma attack is to get your eyes checked regularly, especially if you’re at high risk. Your doctor can keep tabs on pressure levels and how well fluid drains. If they think your risk is unusually high, they may suggest laser treatment to hold off an attack.
