Benign (noncancerous) enlargement of the prostate, known as benign prostatic hyperplasia (BPH for short), is the most common prostate problem in men. Almost all men will develop some enlargement of the prostate as they age.
When Does Prostate Enlargement Happen?
Overall, the number of men with BPH increases progressively with age. Between ages 51 and 60, 50% of men will have some signs of BPH. Up to 90% of men over ager 80 will have signs of this condition. About one-third of these men will develop symptoms that require treatment.
Does BPH Increase Your Risk of Developing Prostate Cancer?
Based on research to date, the answer is no. However, BPH and prostate cancer have similar symptoms, and a man who has BPH may have undetected cancer at the same time.
The American Cancer Society recommends that men make an informed decision with their health care provider whether to be screened for prostate cancer. For men at average risk, this discussion should start at age 50. They also say that for men who are at high risk, such as African-American men and men with a family history of prostate cancer, screening should be considered at age 45. Men at an even higher risk, such as having more than one relative with a history of prostate cancer at an early age, should consider earlier testing.
The American Urological Association recommends against routine screening for men ages 40 - 54 who have an average risk of prostate cancer. Those with a higher risk are encouraged to discuss prostate cancer screening tests with their doctor. The association recommends that men ages 55 - 69 should weigh the risks and benefits of screening and treatment. For those who choose screening, the AUA suggests that they may be screened every two years rather than annually. Tests used to screen for prostate cancer include a blood test for a substance called prostate-specific antigen (PSA) and the digital rectal exam (DRE). The AUA does not recommend PSA screening in men over age 70 or any man with less than a 10-15-year life expectancy.
The U.S. Preventive Services Task Force recommends that a PSA test may be appropriate for some men between the ages of 55 – 69. The group suggests talking to your doctor first to understand the risks and benefits of a PSA test.
What Are the Symptoms of BPH?
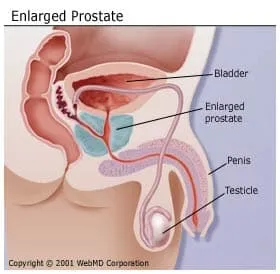
Since the prostate gland surrounds the urethra, the tube that carries urine out of the body, it is easy to see that enlargement of the prostate can lead to blockage of the tube. You may develop:
- Slowness or dribbling of your urinary stream
- Hesitancy or difficulty starting to urinate
- Frequent urination
- Feeling of urgency or sudden need to urinate
- Need to get up at night to urinate
As symptoms progress, you may develop:
- Bladder stones
- Bladder infection
- Blood in your urine
- Damage to your kidneys from back pressure caused by retaining large amounts of extra urine in the bladder
- Sudden blockage of the urinary tube, making urination impossible
How Is BPH Diagnosed?
After evaluating your medical history and giving you a complete physical, your doctor will perform a digital rectal examination.
Because the prostate gland is in front of the rectum, the doctor can feel if the back of the gland has any abnormalities during this examination. This enables the doctor to estimate the size of the prostate and to detect any hard areas that could be cancer.
Several studies may be done to help diagnose your condition:
- A urine test called a urinalysis
- A seven-question BPH Symptom Score Index survey to evaluate the severity of your symptoms
- A flow study to see if the urine stream is slow compared with normal flow
- A study to detect how much urine is left in the bladder after urination
How Is BPH Treated?
Patients with mild symptoms may not require treatment other than watching to make sure their condition doesn't worsen. This approach is sometimes called "watchful waiting" or surveillance. A number of treatment options are available if your symptoms are severe.
Treatments for BPH Include:
- Medication.Finasteride (Proscar) was one of the first drugs used to treat BPH by shrinking the prostate gland. Dutasteride (Avodart) is another similar drug that can be used for the same purpose. They both work by inhibiting the conversion of testosterone to the hormone dihydrotestosterone (DHT), which affects the growth of the prostate gland. These medications appear to be most helpful for men with larger prostates. The FDA has revised labels on Proscar and Avodart to include a warning that the drugs, while capable of reducing overall prostate cancer risk by 25%, may be linked to an increased risk of an unusual type of aggressive or high-grade prostate cancer.
More common are drugs referred to as alpha blockers that relax the muscle in the prostate to reduce the tension on the urine tube. These include alfuzosin (Uroxatral), doxazosin (Cardura XL), silodosin (Rapaflo), tamsulosin (Flomax), and terazosin (Hytrin). Side effects may include light-headedness and weakness. Taking both a DHT inhibitor and an alpha blocker at the same time can be more beneficial at controlling symptoms and preventing the progression of BPH than taking either drug individually.
Other medications may be effective for some men. These may include anticholinergics when symptoms of overactive bladder are present, and PDE-5 inhibitors such as tadalafil (Cialis) if erectile dysfunction is also a problem. - Surgery. A number of surgery types can remove the prostate tissue blocking the flow of urine. The most common is called transurethral resection of the prostate, or TURP. It involves removing the tissue blocking the urethra (urine tube) with a special instrument. Although TURP is effective, side effects may include bleeding, infection, impotence (inability to maintain an erection suitable for sex), and incontinence (inability to control the flow of urine). Another, less complicated procedure is transurethral incision of the prostate (TUIP). Instead of removing tissue, as with TURP, this approach involves widening the urethra by making several small cuts in the bladder neck (area where the urethra and bladder join), as well as in the prostate gland itself. This relieves some of the pressure on the urethra and improves urine flow.
- Minimally invasive treatments. Newer treatments can effectively reduce the size of the prostate and relieve urinary obstruction, but are less invasive and damaging to healthy tissue than surgery. In general, less invasive procedures require less time in the hospital, result in fewer side effects, are less costly, and allow for quicker recovery. Side effects may be urinary frequency and irritation while the prostate is healing. However, many of these techniques are new. Little is known about the long-term effectiveness and complications of these procedures, which include:
- Transurethral Microwave Thermotherapy (TUMT). Microwave energy delivers temperatures above 45 degrees C (113 F) to the prostate by way of an antenna positioned in the prostate using a special catheter (tube). Cool water circulates around the catheter which protects the urethra and helps keep you reasonably comfortable throughout the procedure. The entire procedure is computer-controlled, based on temperature recordings obtained in the urethra and rectum. This technique is performed in your doctor's office and takes approximately 90 minutes. Patients are generally given medicine to prevent pain and relieve anxiety. The most common complaints during the treatment are an urge to urinate and a burning sensation in the penis. There are two programs: "standard treatment" or "high-energy" treatment. High-energy treatment delivers more energy to the prostate, which generally provides better results and improved flow, but patients may have more side effects in the recovery period.
- Interstitial Laser Coagulation. ILC uses a specially designed laser fiber to deliver heat to the interior of the prostate. The laser fiber is inserted into the prostate using instruments placed in the urethra. The procedure is usually done in the operating room, under anesthesia to numb the pain but not put you to sleep. This technique allows the surgeon to view the prostate directly and to treat specific areas of enlargement.
- Transurethral Needle Ablation (TUNA). This technique uses low-level radiofrequency energy delivered through two small needles to ablate, or burn away, an area of the enlarged prostate.
- Transurethral Electrovaporization. This technique uses electrical energy applied through an electrode to rapidly heat prostate tissue, turning the tissue cells into steam. This allows the doctor to vaporize an area of the enlarged tissue and relieve urinary obstruction. Laser photo-vaporization can also be performed.
- Intraurethral stents. Stents (wire devices shaped like springs or coils) are placed within the prostate channel (where the urethra runs through the gland) to help keep the channel from tightening around the urethra.
- Prostatic Urethral Lift. A prostatic urethral lift (PUL) is a permanent implant used to treat BPH. The PUL is placed in the urethra and works by pulling back the prostate tissue that is pressing on the urethra and impeding urine flow. Studies have shown improvement in symptoms in many men for up to five years or more.

