What Is Spinal Stenosis?
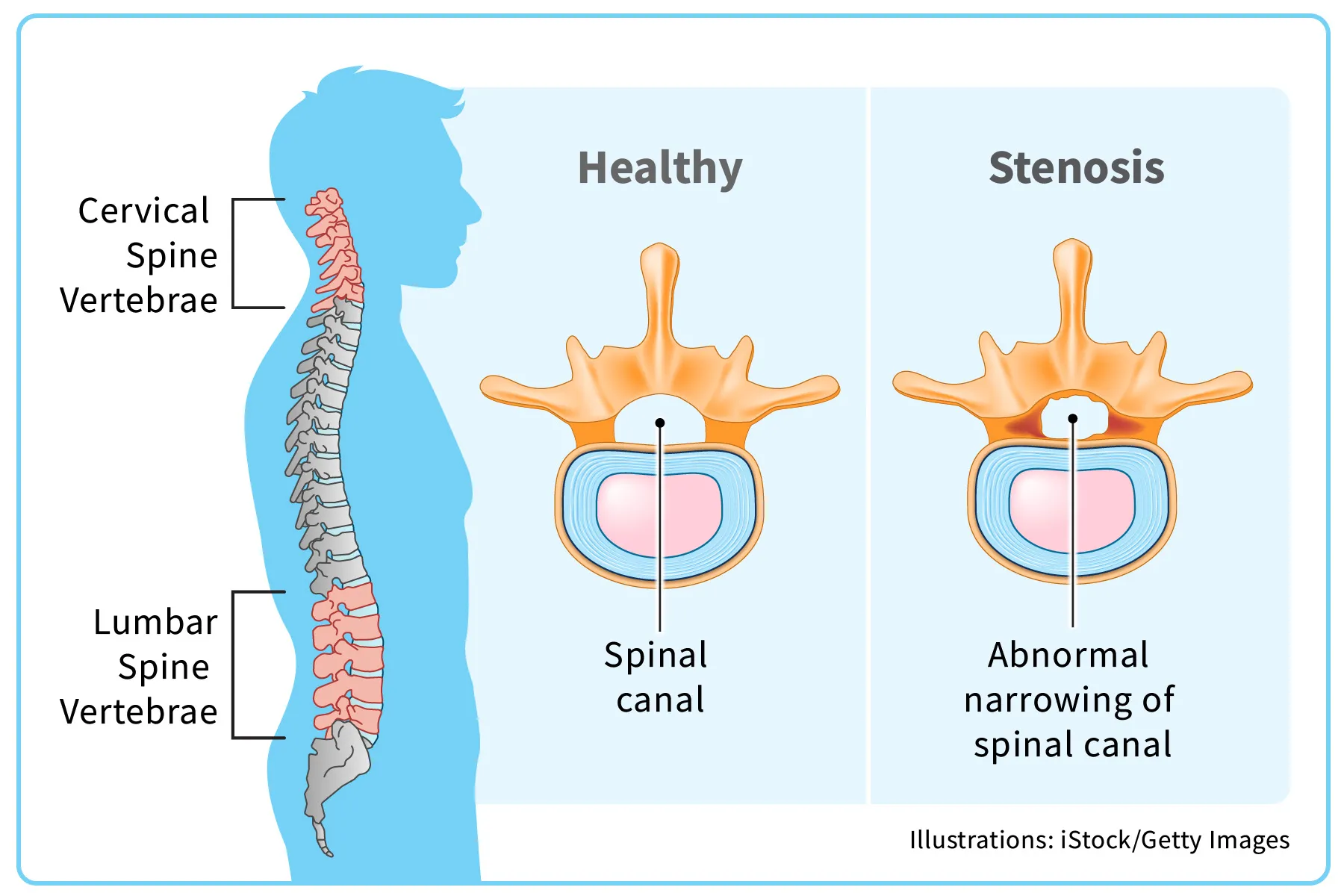
Spinal stenosis is a condition in which open spaces within your spine get narrower. This puts pressure on your spinal cord and the nerves around it, which can cause pain and other problems.
Your spinal cord is a key part of your central nervous system that connects your brain to your body. It rests in the spinal canal, which is formed by the hollow spaces in the center of each vertebra, the interconnected bones that make up your spine. The narrowing can happen in the spinal canal, in the spaces between your vertebrae, or at points where nerves from your spine branch out to other parts of your body.
As these spaces get smaller, the tightness can pinch the spinal cord or the nerves around it, causing pain, tingling, or numbness in your legs, arms, or torso.
Injuries and conditions such as arthritis can lead to spinal stenosis. It's most common in people over 50. There’s no cure, but there are a variety of nonsurgical treatments and exercises to keep the pain at bay.
Types of Spinal Stenosis
There are two main types of spinal stenosis. The type you have depends on where on your spine the condition is:
Cervical spinal stenosis. Cervical stenosisis when the spinal canal in your neck area becomes narrowed.
Lumbar spinal stenosis. You have lumbar stenosis when there's narrowing in the spinal canal in your lower back. This is the most common type.
You can have one or both types of spinal stenosis. You can also have spinal stenosis in your middle back, but this is much less common.
Spinal stenosis and arthritis
For most people, stenosis results from wear and tear on the spine related to arthritis. With osteoarthritis, the cartilage between your joints breaks down. The vertebrae start to rub against each other, which triggers extra bone growth called bone spurs. This extra bone narrows the space within your spinal canal. Arthritis can also cause the ligaments (bands of tissue that hold bones together) in your spine to get thicker, which can make the canal narrower.
Spinal Stenosis Symptoms
Not everyone has symptoms, but if you do, they tend to be the same: stiffness, numbness, and back pain.
More specific spinal stenosis symptoms include:
- Sciatica. This involves shooting pains down your leg that start as an ache in your lower back or buttocks.
- Foot drop. Painful leg weakness may cause you to slap your foot on the ground as you walk.
- Trouble standing or walking. When you’re in an upright position, this tends to compress the vertebrae, causing pain.
- Loss of bladder or bowel control. In extreme cases, spinal stenosis weakens the nerves connected to your bladder or bowel.
- Radiculopathy. This happens when stenosis presses on the root of your spinal nerves, resulting in pain that shoots out from your spine. This causes numbness, tingling, or weakness in your arms and legs.
- Myelopathy. When spinal stenosis squeezes your spinal cord, you may feel numbness, tingling, or weakness in your arms and legs. It can also affect other parts of your body, such as your bladder and bowel.
- Cauda equina syndrome.The cauda equina is a section of nerves at the bottom of your spinal cord. If spinal stenosis compresses this spot, you might lose feeling in your pelvic area, or have problems with bladder or bowel control (incontinence). This can cause permanent nerve damage if you don’t treat it. This is a medical emergency.
If you’re having symptoms, tell your doctor. If you suddenly lose bowel or bladder control and have back pain, get medical help right away.
Spinal Stenosis Causes and Risk Factors
The leading reason for spinal stenosis is arthritis, which is caused by the breakdown of cartilage (the cushiony material between your bones) and the growth of bone tissue.
Other causes include:
- Herniated disks. If one of your disks (the cushions between your vertebrae) gets cracked, material from inside it can seep out and press on your spinal cord or nerves.
- Injuries. An accident may fracture or inflame part of your spine.
- Tumors. If cancerous growths touch your spinal cord, you may get stenosis.
- Paget’s disease. With this condition, your bones grow abnormally large and brittle. This results in a narrowing of the spinal canal and nerve problems.
- Thickened ligaments. When the cords that hold your bones together get stiff and thick, they can bulge into your spinal canal and make it smaller.
Spinal stenosis risk factors
The main risk factor for spinal stenosis is being over 50. Women (and those assigned female at birth) as well as people who've had spinal surgery are at higher risk.
Spinal stenosis risk factors in younger adults
Some people are born with spinal stenosis or diseases that lead to it, such as scoliosis (curvature of the spine). For them, the condition usually starts to cause problems between the ages of 30 and 50. An injury to your spine can also put you at risk for stenosis at a younger age.
Spinal Stenosis Diagnosis and Tests
First steps in spinal stenosis diagnosis
The doctor will probably start by asking questions about your medical history and risk factors. They'll do a physical exam, and may press on areas of your spine to see where you have pain After that, they'll order X-rays or other imaging tests to give them further details about your condition. The tests may include:
Spinal stenosis MRI
An MRI uses radio waves to create a 3D image of your spine. It can show tumors, growths, and even damage to your disks and ligaments.
CT scan for spinal stenosis
A CT scan uses X-rays to create a 3-D image. With the help of a dye injected into your body, it can show damage to soft tissue as well as issues with your bones.
Spinal Stenosis Treatment
There's no cure for this condition. But treatment can help you manage your symptoms. What spinal stenosis treatment you need depends on which part of your spine is affected and how serious your symptoms are. For mild cases, you may not need any treatment. Instead, your doctor will keep an eye on your condition to see if anything changes.
What is the best painkiller for spinal stenosis?
Spinal stenosis medications include a variety of over-the-counter and prescription pain-relieving drugs. Your doctor will determine which is best for you, based on your symptoms and overall health. They'll also consider the possible side effects and complications of pain treatments.
Over-the-counter pain treatment. Common pain remedies such as aspirin, acetaminophen, ibuprofen, and naproxen can offer short-term relief. All are available in low doses without a prescription.
Antidepressants. Taking tricyclic antidepressants, such as amitriptyline, can help ease long-lasting pain.
Corticosteroid injections. Your doctor will inject a steroid such as prednisone into your back or neck. Steroids make the inflammation go down. But because of side effects, they are used sparingly.
Opioids. For short-term pain relief, your doctor might prescribe drugs with codeine, such as oxycodone (Oxycontin, Roxicodone) and hydrocodone (Norco, Vicodin). These drugs can be habit-forming and have serious side effects.
Nerve block. Done with precision, an injection of an anesthetic can stop pain for a certain time.
Muscle relaxants. These can help control muscle spasms.
Anti-seizure medication. You can take these to ease pain from damaged nerves.
Physical therapy. A physical therapist can come up with an exercise routine to build strength and flexibility in your back and core muscles. This can reduce pain and help you move better. They can also teach you less painful ways to do daily activities, such as walking.
Spinal stenosis surgery. If you have a serious case of spinal stenosis, you might struggle to walk or have issues with your bladder and bowels. Your doctor may recommend a type of surgery to create space between the bones so inflammation can go down. You might get:
Laminectomy. This procedure removes the back part of the affected vertebrae.
Laminoplasty. Your doctor puts metal hardware in your neck vertebrae to form a bridge within the open section of your spine.
Laminotomy. The doctor removes a part of your vertebrae to relieve pressure.
Minimally invasive surgery. This type of surgery helps avoid spinal fusion by removing bone tissue in a way that reduces damage to nearby healthy tissue.
Decompression procedure. The doctor uses needle-like instruments to remove part of the thickened ligaments in your spinal column. You get this procedure only if you have lumbar spinal stenosis caused by thickened ligaments.
Spinal fusion. A surgeon permanently fuses two of your vertebrae together. This operation is considered a last resort and used only if no other treatments have helped. While it can help ease pain, it limits your mobility.
All surgery options carry some risks. Talk to your doctor about how much it can help you, recovery time, and more.
What is the newest treatment for spinal stenosis?
One newer treatment option for spinal stenosis involves placing a spacing device called aninterspinous spacerbetween your vertebrae. The doctor makes a tiny cut in your back, inserts the device through a tube, then expands it once it's in place. You don't need to go to the hospital for this minimally invasive procedure.
Another is a joint replacement operation called the Total Posterior Arthroplasty System (TOPS). A doctor implants a device that stabilizes your spine but doesn't restrict your movement like spinal fusion.
Researchers are also looking at stem cell therapy to treat spinal stenosis. For this treatment, a doctor collects stem cells -- cells that can develop into any type of cell -- from your body. They inject the stem cells into the damaged area of your back, where they help generate healthy tissue.
Early results show promise, but we need more research into this treatment.
Spinal Stenosis Home Remedies
Some things that can help ease symptoms include:
Spinal stenosis exercise. Regular exercise helps you maintain mobility. Your physical therapist can give you stretching and strength exercises, tailored to your needs, to do at home. If your doctor says it's OK, add moderate cardio exercise such as walking, swimming, or riding a stationary bike.
Apply heat and cold. Heat boosts blood flow, loosens muscles, and soothes joints. Cold reduces inflammation. Try a hot or cold pack on your neck or lower back and see what works best for you. Hot showers are also good.
Posture. Stand up straight, sit on a supportive chair, and sleep on a firm mattress. And when you lift heavy objects, bend from your knees, not your back.
Weight loss. Because extra pounds put added pressure on your back, losing them may improve your symptoms.
Assistive devices. Braces, a corset, or a walker could help you get around, provide stability, and reduce pain.
Alternative medicine for spinal stenosis
Along with medical treatment, many people try nontraditional therapies such as chiropractic care, acupuncture, and massage therapy. Let your doctor know if you’re trying an alternative approach.
Spinal Stenosis Complications
If you don’t treat spinal stenosis, it can get worse over time. Certain symptoms may even become permanent, including:
- Numbness
- Weakness
- Problems with balance
- Loss of bladder and bowel control
- Paralysis
Living With Spinal Stenosis
Spinal stenosis affects different people in different ways. Most people with the condition don't need surgery and are able to live active lives, though they may need to make some changes to the way they work or exercise.
To keep your back as pain-free as possible:
- Do some kind of moderate exercise every day. Activities in which you lean forward, such as walking on a treadmill with an incline or using a step climbing machine, can ease pressure on your back. Exercises done in water can help, too.
- Reach and maintain a weight that's healthy for you.
- Try not to stay in one position for too long.
- Sit down whenever you need to.
- Learn to move in ways that don't hurt your back.
Things to avoid with cervical spinal stenosis
Stay away from or modify activities that could lead to pain or injuries. It's best to avoid:
- Lifting heavy items
- High-impact activities such as running or jumping
- Contact sports
- Bad posture
- Repetitive movements such as texting or typing without frequent breaks
- Smoking (ask your doctor if you need help quitting)
Takeaways
With spinal stenosis, open spaces within your spine get narrower and pinch your spinal cord and the nerves around it. This can cause pain, numbness, and other issues. There's no cure, but treatment and lifestyle changes can help you manage the symptoms.
Spinal Stenosis FAQs
What are the stages of spinal stenosis?
Imaging tests can help your doctor see how serious your condition is. When they look at your MRI results, they can determine whether your spinal stenosis is:
- Stage 0: No stenosis (narrowing) of the spinal cord
- Stage I: Mild stenosis
- Stage II: Moderate stenosis
- Stage III: Severe stenosis
What are the final stages of spinal stenosis like?
Symptoms of the later stages can include:
- Numbness in your legs, feet, or groin and upper thigh area
- Trouble standing or walking
- Leg pain when you move
- Loss of bladder or bowel control
You may need surgery if your stenosis is in an advanced stage.
What does spinal stenosis leg pain feel like?
If you have spinal stenosis, you might have leg pain that feels like prickling or burning. It may start in your buttocks and spread down to your feet. You might also have cramps, numbness, or weakness in your legs. The symptoms often start or get worse when you stand, walk, or exercise. They may improve when you crouch down or lie in a fetal position.
How do you stop spinal stenosis from progressing?
You can't necessarily stop spinal stenosis from progressing. But you can slow it down with treatment and by taking steps such as exercising regularly, maintaining a healthy weight, and avoiding activities that could lead to further spine damage. Spinal stenosis tends to progress very gradually over many years.
What is the life expectancy of someone with spinal stenosis?
Spinal stenosis doesn't affect your life expectancy, though it can cause disability if you don't get treatment or take other steps to manage symptoms and maintain your mobility.

