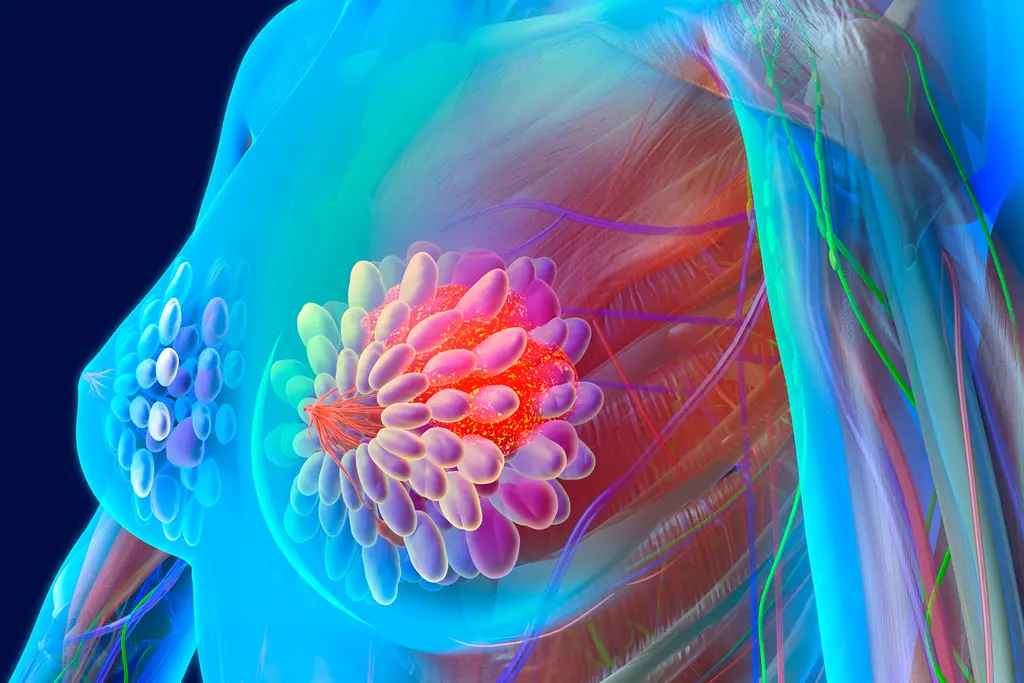
You've just been diagnosed with HER2+ breast cancer, and you're wondering what happens next. Every person is different, but here’s what treatment generally looks like and what milestones you can expect.
After Your Diagnosis
Depending on what stage your cancer is in, your health care team will come up with a treatment plan that's best for you. This could include:
- Surgery
- Radiation therapy
- Chemotherapy
- Drugs known as targeted therapies
Usually, the more your cancer has spread, the more treatment you will need. HER2+ cancers tend to grow and spread faster than other types of breast cancer, but they are also more responsive to drug treatment. Keep in mind that your progress may not always go in a neat series of steps.
Surgery
This is usually the first step in the treatment of early breast cancer (stages I and II). Depending on where your tumor is and the size of your breast, you may be able to get breast-conserving surgery (also known as a lumpectomy). This aims to leave as much of your breast intact as possible. You'll often be left with a small scar and indentation. Usually, you’ll get radiation therapy after the operation.
If you're not able to have radiation therapy (maybe you're pregnant or you have a condition like lupus that makes it difficult to tolerate the side effects of radiation), your doctor may suggest a mastectomy. This is surgery to remove the entire breast. Different types of mastectomies are available that can preserve your skin and nipple. This will help if you decide to reconstruct your breast later.
During surgery, the surgeon will also remove some of your lymph nodes and send them for testing to see if your cancer has spread.
If you get breast-conserving surgery, you’ll usually have it in an outpatient center. You can go home the same day. If you get a mastectomy, you will usually stay in the hospital for 1-2 nights.
Because stage III breast cancer tumors are larger, it's likely you'll start with chemotherapy plus targeted therapies that target the HER2 receptor. The idea is to try to shrink the tumor before surgery. If this works, you may be able to get breast-conserving surgery. If not, your doctor will probably recommend a mastectomy. You’ll usually get radiation afterward. Then you’ll take more targeted therapy drugs for up to a year.
Stage IV cancer has spread beyond the breast and lymph nodes to other parts of the body, like the bones, liver, and lungs. There isn’t a cure, so your treatment will focus on easing your symptoms and prolonging your life. For this reason, surgery is usually not a go-to treatment.
Radiation Therapy
This uses high-energy X-rays, gamma rays, or another type of radiation to kill cancer cells, including any that may have been left behind after surgery. The most common type of radiation is called external beam radiation. This is when a machine aims radiation at a specific part of your body. Your doctor will carefully plan the exact dose and the area to apply it. The goal is to kill as many cancer cells as possible without harming healthy ones. Most people get 10-20 minutes of radiation therapy 5 days a week for 3-7 weeks. The procedure itself is painless, but side effects include pain, swelling, and fatigue.
Your doctor will almost always recommend radiation after breast-conserving surgery. You may not need it after a mastectomy if there's no cancer in your lymph nodes.
For stage IV cancer, your doctor will sometimes use radiation therapy to help make you more comfortable. For example, it can target an area of cancer that is pressing on your spinal cord.
Drug Therapy
There are a range of drugs known as targeted therapies or targeted drugs that work specifically on HER2+ cancer. In many cases, people with stage I, II, or III cancer get a medication called trastuzumab (Herceptin), either with or without chemotherapy. Along with this drug, or possibly instead of it, you may get another targeted drug called pertuzumab (Perjeta). There are also several drugs that are biologically similar to trastuzumab that are approved by the FDA.
You’ll usually get these treatments as an IV drip, but trastuzumab and hyaluronidase (Herceptin Hylecta), and trastuzumab, pertuzumab, and hyaluronidase (Phesgo) are treatments that you’ll get as a shot under your skin.
Kinase inhibitors are another type of targeted therapy that block HER2 and other kinase proteins that help cancer cells grow. Neratinib (Nerlynx) is a pill that you take every day by mouth.
After surgery, you'll take these drugs for up to a year. Sometimes, your doctor will have you start taking them right before surgery, too. If you need more treatment, your doctor may put you on neratinib for an additional year.
If you have stage IV cancer, trastuzumab could help you live longer when you get it along with other medications. Other targeted drugs your doctor might use include pertuzumab, lapatinib, and ado-trastuzumab emtansine (Kadcyla).
Follow-Up Care
Once you've finished treatment, your doctor will probably schedule follow-up visits every few months. After 5 years, you'll go in about once a year. Your doctor will help you come up with what's called a survivorship care plan. This plan will include
- Any future tests you'll need
- Long-term side effects to watch out for
- Suggestions for diet, exercise, and lifestyle changes to help you feel your best
Show Sources
Photo Credits:
Header Image: NADOFOTOS / Getty Images
Inset 1: gorodenkoff / Getty Images
Inset 2: Thomas Hecker / Getty Images
Inset 3: Nattapong_Choudram / Getty Images
SOURCES:
American Cancer Society: "Treatment of Breast Cancer Stages I-III," "Targeted Therapy for Breast Cancer," "Breast Cancer HER2 Status," "Breast-conserving Surgery (Lumpectomy)," "Mastectomy," "Treatment of Stage IV (Metastatic) Breast Cancer," "Radiation for Breast Cancer."
Susan G. Komen: "Assessing Lymph Nodes," "Going Through Radiation Therapy."
American Society of Clinical Oncology: “ASCO Cancer Treatment and Survivorship Care Plans.”