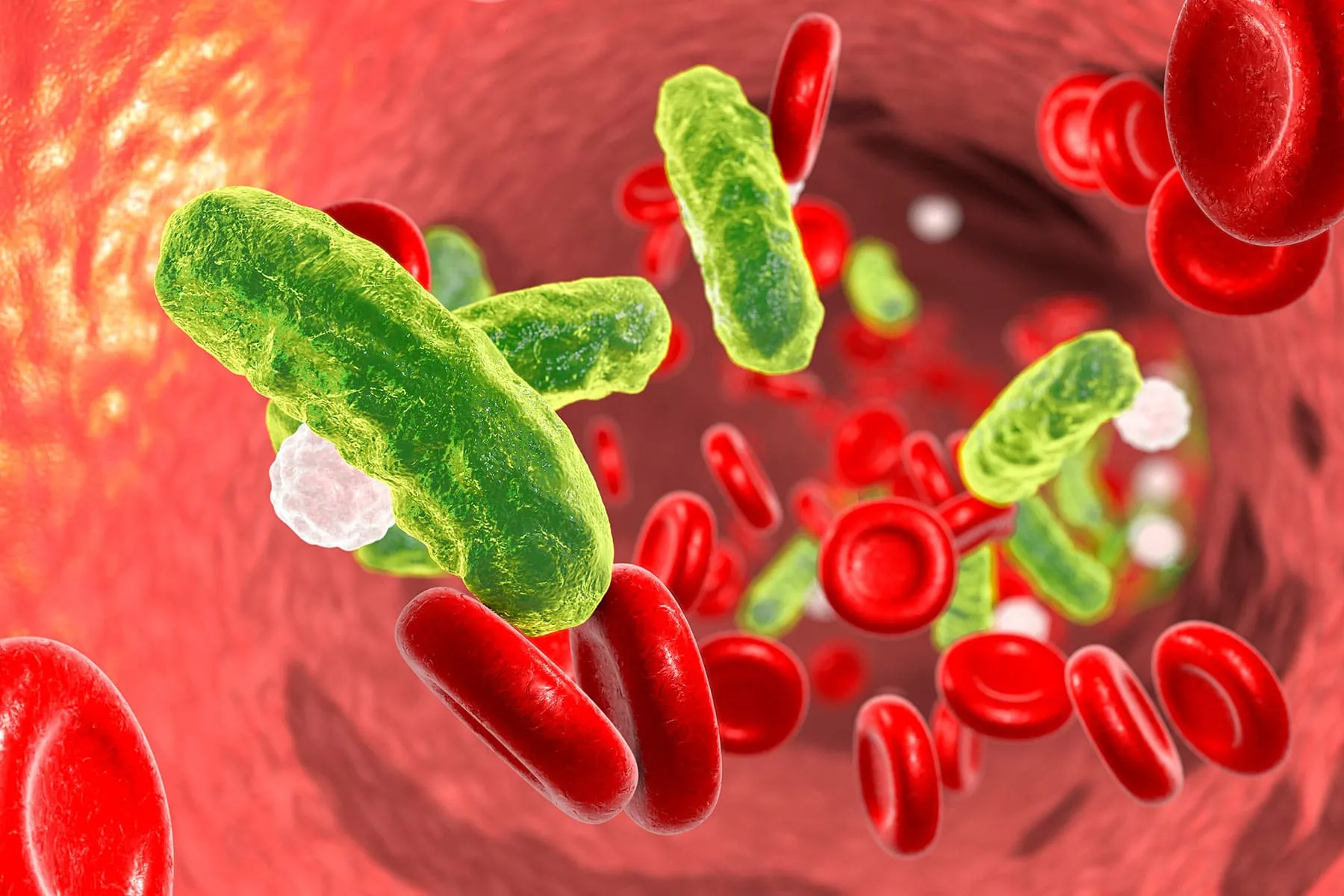
Sepsis may not be on your radar but it is an extremely deadly killer.
Worldwide, a stunning one-third of people who get it die, and many who do live have life-changing side effects such as chronic pain and fatigue, organs that don’t work well, even amputations. Sepsis is caused by a bacterial infection, and many conditions can lead to it. You can be completely healthy or have a condition that makes you more likely to get it.
One very susceptible group: children.
While sepsis overwhelmingly strikes the elderly -- up to 85% of all cases are in seniors -- more than 75,000 children develop sepsis annually in the United States, according to the Sepsis Alliance. Seven thousand die.
Doctors are hoping to cut down on those deaths by educating themselves and parents about the symptoms, which can be vague and difficult to recognize. They can also vary drastically child to child, says Niranjan Kissoon, MD, vice chair of the Global Alliance for Sepsis and a member of the Sepsis Alliance advisory board.
Kissoon is working with the CDC to gather data on sepsis. He says one of the biggest barriers is accepting that sepsis is a major public health issue. “In the United States, more than 18 children die from sepsis each day, and this is tragic in the sense that many of these lives could be saved with improved public awareness of the symptoms and expanded health care provider education and early treatment,” says Kissoon, a professor of pediatrics and emergency medicine at the University of British Columbia. He says it causes more deaths than cancer.
The social and economic disparities are also troubling and must be addressed, he adds. “Studies have shown that preterm infants who are black are 13 times more likely to develop sepsis and 15 times more likely to die than infants who are not black,” he says. “Infants of low-income families are 20 times more likely to die of sepsis. In fact, infants from families without insurance are also three times more likely to die.”
A Close Call
Marnie Doubek, MD, struggled for several days to figure out what was wrong with her son Zachary when she found him crying one night after a baseball game in 2014. “He said he had a headache and he was dizzy and his knee hurt,” Doubek says. She and her husband, Joe, thought maybe Zach, who was 11 at the time, hurt his knee sliding into a base. The next morning, he still had knee pain. Doubek gave him some ibuprofen, and about an hour later, he felt well enough to go to school. But that was short-lived. It would take nearly a week and multiple doctors before Zach was diagnosed with sepsis.
“I got a call from the school nurse. He was limping and saying that his knee hurt,” Doubek recalled. “She said he didn’t have a fever, but what she did say to me was, and this is a quote from her, ‘He just doesn’t look right.’”
The next day, Doubek, a primary care doctor in Maplewood, NJ, took Zach to be seen by one of her associates. She thought there was a chance Lyme disease might be the culprit, so she drew some blood and started him on the antibiotic amoxicillin.
When the bloodwork came back, and a marker for inflammation was critically elevated, they went to see an orthopedist. Doubek says she was starting to freak out, and Zach was looking pretty sick. The orthopedist thought it might be inflammation of the lining of the joint. But Zach got worse. By the next evening, he was in such agony, he could barely move. And then, Doubek says, he became delirious.
“It was about 3 o’clock in the morning and he asked me for water,” Doubek remembers. “I picked up the water bottle and went to hand it to him. He looked at me and said, ‘Is someone going to fly it to our house?’” She took Zach to the local emergency room, where doctors transferred him to a hospital with a pediatric intensive care unit.
“They did not have a clear idea of what was going on at that point,” Doubek says. “No one specifically said, he’s septic or has sepsis. They were wondering if he had some kind of tick-borne illness. Nobody really knew, but they knew that he was in respiratory failure, he was in liver failure, and he was in kidney failure.”
Once in the ICU, Zach was given broad-spectrum antibiotics and put on a respirator. Doubek says 2 days later, his doctors determined Zach had osteomyelitis, a bone infection of his right femur. He was rushed to surgery to drain the infection.
“He stayed on that respirator unconscious for about 2 weeks, in and out of surgery with high fevers. He was on medication to keep his blood pressure up. There were multiple complications. He had a lung collapse, and even required a chest tube. Finally, after about 2 weeks of pure hell, he started to do a little bit better.”
“It was hard to believe that our healthy 11-year-old son, who had been playing baseball four days earlier, was on a respirator, sedated, and asleep. He had IV lines and a catheter. You walk into the room and you cannot believe what has just happened,” Doubek says.
Improving the Odds
Kissoon says one critical problem with sepsis is making a diagnosis. “The signs and symptoms initially can be very subtle, and many a time, we misdiagnose children and we think they have a common cold,” he says.
There are no tests that can give you a diagnosis of sepsis immediately, Kissoon says. He says if doctors suspect sepsis, they start antibiotics right away rather than wait until the diagnosis is confirmed.
Most doctors agree that an hour can make all the difference.
“Sometimes children have pre-existing conditions that make them susceptible to infections and ultimately sepsis,” says Michael Bell, MD, chief of critical care medicine at Children’s National Hospital in Washington, DC. “But other times, it is just terrible luck that happens to some kids where they get overwhelmed by an infection and can lead to quite a difficult hospitalization and rehabilitation.”
Lauren Hess, MD, co-lead of a sepsis quality improvement project at Texas Children’s Hospital in Houston, says children are also more vulnerable because many of the common conditions they have can lead to sepsis.
And younger children may not be able to express how they’re feeling, says Charles Macias, MD, chief of the Division of Pediatric Emergency Medicine at University Hospitals Rainbow Babies & Children’s Hospital in Cleveland, OH.
Kissoon says there is another critical issue facing children like Zach who survive sepsis.
“One-third of those who are discharged from hospital will have some form of disability, either physical impairments, cognitive difficulty, skin graph, amputations, hearing loss; some suffer even things like almost post-traumatic stress disorder,” he says. “So sepsis is a major problem -- long term. I think when we talk about death, it is really the tip of the iceberg because these children have life-long issues, and more than 20% of child sepsis survivors are readmitted to the hospital within 3 months of the initial hospitalization.”
Three years ago, Texas Children’s Hospital in Houston joined a group of more than 50 other children’s hospitals working toward improving sepsis care.
An early warning system uses an electronic health record to look at the patient’s vital signs and history to help flag the bedside care provider if the patient could be getting sepsis, Hess says.
Terri Brown, RN, says the new systems at Texas Children’s have helped cut its mortality rate from sepsis. “We have seen a 36% relative reduction in our 3-day mortality, and we have much more of a sense of urgency, really hitting that golden hour of assessment and intervention.”
Children’s in Washington, DC., uses “sepsis charts” containing education materials on its units. The goal is to educate staff about early recognition and treatment -- particularly about giving antibiotics at the earliest possible time, Bell says, along with more invasive treatments such as IV fluids. Children also may be put on a ventilator if they need help breathing.
Bell is also part of the collaborative pediatric critical care research network, a National Institutes of Health-funded group of investigators doing research on a number of topics related to critically ill kids, including sepsis.
Still, it’s a challenge.
“It has been an aspiration for decades to have a medication or drug that can be administered to all children with sepsis that will mitigate the secondary effects of the infection,” Macias says. “Sadly, none of these ‘magic bullets’ has proven to be effective in large clinical trials.”
He says the sheer number of annual cases cost an astonishing amount of money. “There’s tremendous financial burden associated with sepsis,” Macias says. “Likely over $4.5 billion a year in health care costs.”
But he says the efforts of hospitals all over the country have led to “considerable improvements” in care and outcomes.
“Almost 20% more children are being recognized as having sepsis” -- critical because timely recognition and interventions with fluids and antibiotics are keys to reducing deaths and severe side effects, Macias says.
These improvements have also led to a decrease in the length of hospital stays and sepsis-related mortality at the hospitals in the Improving Pediatric Sepsis Outcomes collaborative, he says.
Zach Doubek’s Future
Zach, while one of the lucky ones, will have lifelong complications from his fight with sepsis.
He had permanent damage to the nerves in one leg. As a result, that leg did not grow the same, so he wears a lift in his shoe. He also has a weakened calf muscle, less sensation in his foot, and issues with focusing and anxiety.
“Overall, he’s done amazingly well, he’s come so far -- but the truth is he’s still on the journey,” Marnie Doubek says. “It doesn’t have an ending yet. It’s been a rough 5 years for him. It’s been a process of redefining himself.”
While Zach figures out who he is, his mother is on a mission to make sure sepsis is on everyone’s radar so that what happened to her son does not happen to someone else’s. She plans to continue speaking out to get the message across to other families.
“I do it because I am so grateful. I know how easily it could have gone the other way. There were such moments of intense fear that he wasn’t going to make it -- it’s a very dark, scary place to be so close to, so yeah, we’re very lucky. I know there are many, many families that unfortunately can’t say the same thing.”
Spotting Sepsis
Some signs of sepsis that may appear in a child of any age:
- Feels abnormally cold to the touch
- Looks mottled, bluish, or has very pale skin
- Has a rash that does not fade when you press it
- Is breathing very fast
- Has a convulsion
- Is very lethargic or difficult to wake up
Some additional signs for children younger than age 5:
- Not eating
- Repeated vomiting
- Not urinating for 12 hours
Find more articles, browse back issues, and read the current issue of WebMD Magazine.
