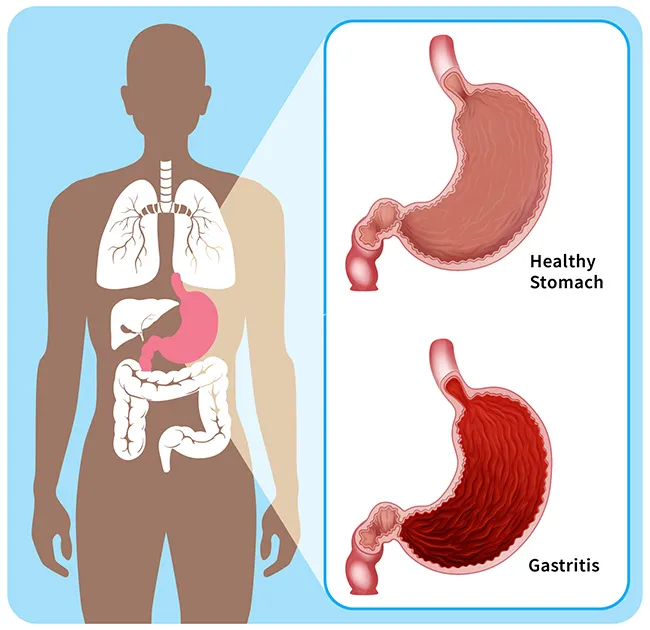
Gastritis is an inflammation, irritation, or erosion of the stomach lining. It can come on suddenly and last a short time (acute), or start gradually and be long-lasting (chronic).
It's a common condition, affecting about 8 in every 1,000 people in the U.S. The acute form is often caused by an infection, too much alcohol, or medications that irritate the stomach. . Across the world, up to half of the population is thought to have chronic gastritis linked to infection with the Helicobacter pylori (H. pylori) bacteria.
Types of Gastritis
In addition to the acute and chronic forms, gastritis can be divided into types based on how it affects the protective lining of your stomach.
Erosive gastritis. With this type, whatever causes gastritis leaves injuries or ulcers in your stomach lining.
Nonerosive gastritis. People who have this type have stomach irritation but no ulcers. If you have a type of nonerosive gastritis called atrophic gastritis, the irritation causes your stomach lining to get thinner.
Doctors may also identify gastritis by what causes it, such as:
- Alcohol-induced gastritis
- Autoimmune gastritis
- Drug-induced gastritis
- Infectious gastritis
- Stress-induced gastritis
What Causes Gastritis?
Gastritis is your body's response to weakness or damage in your stomach lining. Many things can lead to it, including:
- Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or naproxen
- Overuse of alcohol, tobacco, or cocaine
- Repeated vomiting
- Stress, such as that caused by an injury, surgery, or serious illness
- Infections caused by bacteria such as H. pylori
- Other infections, including parasitic infections, HIV/AIDS, and the viruses that cause "stomach flu"
- Bile reflux, in which a digestive fluid called bile backs up into your stomach
- An autoimmune response in which your immune system attacks the cells of your stomach lining
- Inflammatory conditions such as Crohn's disease, celiac disease, or sarcoidosis
- Chemotherapy and radiation treatments
Because the stomach lining tends to get thinner with age, older people are at higher risk for gastritis.
Gastritis Symptoms
Symptoms of gastritis vary from person to person, and many people don't have any. Gastritis symptoms may include:
- Indigestion, a burning or gnawing feeling in your stomach that tends to happen between meals or at night
- Nausea and vomiting
- Bloating in the belly area
- Stomach pain
- Hiccups
- Appetite loss
If gastritis has caused a bleeding ulcer, you might:
- Vomit blood or coffee ground-like material
- Have poop that looks black and tarry
Gastritis Tests
To diagnose gastritis, your doctor will review your personal and family medical history and do a physical exam. They may also recommend any of the following tests:
Upper gastrointestinal (GI) series or barium swallow. This is an X-ray that gives your doctor a look at the upper part of your digestive system. Before the X-ray, you swallow a chalky liquid called barium. It coats your organs to help your doctor see them. It can reveal whether there's erosion in your stomach lining.
Upper endoscopy. An endoscope, a thin tube containing a tiny camera, is inserted through your mouth and down into your stomach to check your stomach lining for signs of inflammation . At the same time, they may also do a biopsy, in which they remove a tiny sample of tissue and send it to a lab for analysis.
Blood tests. The doctor may check your red blood cell count to see whether you have anemia, which is when you don't have enough red blood cells. They can also use blood tests to screen for H. pylori infection and pernicious anemia.
Fecal occult blood test (stool test). This test checks for the presence of blood in your poop, a possible sign of gastritis.
Breath test for H. pylori. You may have this test if your doctor thinks you may be infected with the H. pylori bacteria. You swallow a substance called urea, which the bacteria break down into carbon dioxide. You breathe into a bag, and the breath sample is tested for excess carbon dioxide.
Gastritis Treatment
Gastritis treatment depends on what's causing it and how serious it is.
Acute gastritis may go away on its own, or get better when you stop smoking, drinking alcohol, or taking certain drugs. If you have an alcohol or drug use disorder, your doctor can refer you to treatment programs. If NSAIDs are causing your gastritis, they can suggest alternative pain medications. If you have chronic gastritis, you'll need treatment to cure it permanently.
Gastritis medications may include:
Antacids. These are medications you can buy over the counter to ease indigestion and heartburn. They work by neutralizing stomach acids. There are many different types, including Maalox, Mylanta, Rolaids, and Tums. Talk to your doctor or pharmacist about what kind to take, and avoid those that contain aspirin.
H2 blockers. Histamine-blocker (H2) drugs, available either over the counter or by prescription, reduce how much acid your stomach produces. They include cimetidine (Tagamet), famotidine (Pepcid), and nizatidine.
Proton pump inhibitors. These drugs help block stomach acid production. They're also available over the counter or by prescription. These include dexlansoprazole (Dexilant), esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), and rabeprazole (Aciphex).
Surface coating agents. These prescription drugs protect damaged stomach tissue from acid and enzymes so it can heal. They include sucralfate (Carafate) and misoprostol (Cytotec).
Antibiotics. If your gastritis is caused by a bacterial infection, such as H. pylori, your doctor will likely prescribe antibiotics along with medications to reduce stomach acid.
Anti-nausea medications. If you have nausea as a result of gastritis, you can take over-the-counter or prescription medications to ease this symptom.
If an autoimmune disorder is causing your gastritis, your doctor can prescribe medications to treat that disorder. For autoimmune gastritis, they might recommend supplements of Vitamin B12, folic acid, or iron.
If you have bile reflux or gastrointestinal (GI) bleeding, your doctor may suggest surgery to repair the problem. But this is uncommon.
Gastritis Complications
Gastritis usually doesn't cause long-term problems. But when it damages your stomach lining, complications can result, such as:
Peptic ulcers. These painful sores in your stomach lining can cause bleeding and scarring.
Gastric outlet obstruction: Scar tissue from ulcers or long-term inflammation can partially or fully block the opening between your stomach and intestine. This can hinder digestion and cause pain, nausea, and vomiting.
Gastrointestinal perforation. An ulcer can eventually turn into a hole (perforation) in the wall of your stomach. This, in turn, could lead to an infection in your abdominal cavity called peritonitis.
Anemia. Iron-deficiency anemia could result from blood loss due to bleeding ulcers or due to continued irritation of your stomach lining. It can also be caused by H. pylori infection or autoimmune gastritis, both of which keep your body from absorbing iron as well as it should. Gastritis may also lead to pernicious anemia, in which your body can't absorb enough Vitamin B12.
Atrophic gastritis. Even nonerosive gastritis can lead to complications over time. The mucus layer in your stomach lining can get thinner and won't work as well as it should. Your body may not be able to properly absorb nutrients such as vitamin B12, folic acid, and iron. This can lead to nutrient deficiencies and anemia.
Achlorhydria orhypochlorhydria. Atrophic gastritis sometimes keeps your stomach from making enough (hypochlorhydria) or any (achlorhydria) hydrochloric acid, a component of stomach (gastric) acid. This can interfere with digestion and keep your body from absorbing enough nutrients.
Gastric intestinal metaplasia. This is a rare condition in which chronic gastritis leads to changes in the cells of your stomach lining, increasing your risk for stomach cancer.
Stomach cancers. Atrophic gastritis raises your risk for adenocarcinoma of the stomach as well as mucosa-associated lymphoid tissue (MALT) lymphoma and neuroendocrine tumors.
Gastritis Prevention
These things may help you avoid gastritis, or keep your symptoms from getting worse if you have it:
Good hygiene. H. pylori can be passed from person to person or in contaminated food or water. The most important way to keep it from spreading is to wash your hands often, especially after you use the restroom and before you handle food.
Stop smoking. Smoking raises your risk for infection with H. pylori and for peptic ulcers.
Limit alcohol. Because alcohol can irritate your stomach lining and make it more prone to damage, drink it in moderation if you drink it at all.
Don't overuse NSAIDs. NSAIDs such as aspirin, ibuprofen, and naproxen can also irritate your stomach lining. Don't use them for long periods or at high doses. See your doctor if you need other pain-relief options.
Manage stress. Since stress may contribute to gastritis, look for healthy ways to handle it. Relaxation techniques, such as mindfulness meditation, tai chi, or yoga, may help.
Avoid foods and drinks that could irritate your stomach lining. Things such as coffee and spicy and greasy foods don't cause gastritis, but they could make your symptoms worse if you already have it.
What Is the Prognosis for Gastritis?
The outlook for people with gastritis depends on the cause of their illness. An occasional case of acute gastritis will likely get better on its own.
If you often have gastritis or it won't go away, see a doctor. Medication or changes to your lifestyle will most likely improve your symptoms. If you have trouble quitting smoking or have a substance abuse disorder, your doctor can recommend techniques and programs to help you succeed.
If another condition is causing your gastritis, successfully treating that condition should also improve your stomach issues.
Takeaways
Gastritis is irritation of your stomach lining. It's often caused by an infection or by the overuse of alcohol tobacco or over-the-counter pain relievers. An occasional case will probably go away without treatment, but long-lasting (chronic) gastritis should be treated by a doctor.
Gastritis FAQs
How do I get gastritis to go away?
The best way to get rid of gastritis is to deal with whatever caused it. You might need to stop smoking or cut down on alcohol or over-the-counter painkillers. Or you may need to be treated for an infection or other condition that is causing your symptoms or making them worse.
How long does gastritis last?
Acute gastritis may last a few days. Chronic gastritis can last months or even years.
What foods are good for gastritis?
There's no such thing as a gastritis diet because experts don't think diet plays a role in most cases of gastritis. But drinking too much alcohol can cause it, as can eating a food you're allergic to.
How to ease gastritis pain fast?
Antacids can quickly ease the pain of gastritis by neutralizing stomach acids. But they don't address its causes.
What to eat when you have gastritis?
When you have symptoms, it may be best to limit:
- Alcohol
- Caffeine
- Sodas
- Spicy and fatty foods
- Acidic foods such as citrus fruits
To help digestion, eat more frequent and smaller meals. Focus on less-processed foods such as fruits and veggies, nuts and seeds, beans, eggs, and small amounts of poultry and lower-fat meats.
Listen to your body, and notice whether any foods affect your symptoms. Keeping a food diary can help you figure this out. Your doctor or a dietitian can give you diet recommendations based on your own needs and medical history.
