What Is Heart Failure?
Heart failure is when your heart can't pump enough blood to provide your body with the blood and oxygen it needs. If you have this condition, it doesn't mean your heart stops working. It means your heart doesn't work as efficiently as usual. Blood moves through your heart and body at a slower rate, and pressure in your heart raises.
The condition affects nearly 7 million Americans. About 1 in 4 people will get diagnosed with it in their lifetime. Heart failure is the main reason why people older than 65 go to the hospital.
Heart failure pathophysiology
Pathophysiology is the process that leads to heart failure. When your heart doesn't pump strongly enough, your body adapts so it can meet your body's need for blood.
The chambers of the heart may stretch so they can hold more blood to pump through your body. Or the heart muscle gets stiff and thicker to keep the blood moving. Over time, the extra work causes cells in the heart to die. The heart muscle walls get weaker and are less able to pump.
When your heart doesn't work well, your body releases hormones that narrow your blood vessels and make your kidneys hold onto more fluid (water) and salt. The extra fluid and salt raise your blood pressure and make your heart work even harder. Fluid builds up in your arms, legs, ankles, feet, lungs, or other organs. Doctors call this condition congestive heart failure.
In time, your heart gets so weak that it can't pump enough blood to meet your body's needs. That's heart failure.
Heart failure vs. heart attack
Heart failure is different from a heart attack.
During a heart attack, a blood clot or the buildup of a sticky substance called plaque in your arteries blocks blood flow to your heart. Without oxygen, part of the heart muscle begins to die. You need quick treatment to open up the blocked blood vessel and restore blood flow to the heart.
Heart failure is a slower process. Your heart gradually becomes damaged from working too hard. Over time, it becomes less able to pump enough blood out to meet your body's needs.
What Causes Heart Failure?
Heart failure is caused by many conditions that damage the heart muscle, including:
- Coronary artery disease (CAD). CAD happens when sticky plaque builds up in the arteries that supply blood and oxygen to the heart. Blood flow to the heart muscle drops. If the arteries become blocked or severely narrowed, the heart is starved for oxygen and nutrients.
- Heart attack. A heart attack is a sudden blockage in an artery that sends blood to the heart muscle. Without blood, part of the heart muscle becomes damaged and doesn't work the way it should.
- Cardiomyopathy. Damage to the heart muscle prevents it from pumping enough blood. Gene changes, infections, and alcohol or drug use can cause this condition.
- Conditions that overwork the heart. High blood pressure, heart valve disease, thyroid disease, kidney disease, diabetes, or heart problems you're born with can cause heart failure. Sometimes, more than one disease combines to cause heart failure.
Heart Failure Symptoms
You may not have any symptoms of heart failure. If you do have symptoms, they might be constant or come and go. They can be so mild you barely notice them or severe enough to affect your daily life.
Early signs of heart failure in adults
Look for these five early warning signs of heart failure:
- Tiredness. You'll feel extra tired if your heart doesn't get enough oxygen.
- Shortness of breath. A drop in oxygen-rich blood could make it hard to catch your breath.
- Cough or wheezing. These symptoms are from fluid buildup in your lungs.
- Swelling. A weak heart can't pump blood back up from the lower part of your body. Fluid can collect and cause swelling called edema in your ankles, legs, and belly.
- Trouble doing activities. Fatigue and shortness of breath can get in the way of your daily routine and make it hard to exercise.
Other heart failure symptoms include:
- Raised need to pee at night from extra fluid in your body
- Appetite loss or nausea from bloating in your stomach
- Dizziness or confusion from a lack of blood to your brain
- Weakness because you have less blood flow to your muscles
- Fast or irregular heartbeat as your heart tries to pump more blood to your body
- Fast weight gain from fluid buildup
- Chest pain if a heart attack caused the heart failure
Heart Failure Types
Heart failure can affect the left side of the heart, the right side of the heart, or both sides. Doctors also classify heart failure based on how well the heart can still pump.
Left-sided heart failure. This is the most common type. The left side of the heart, called the left ventricle, does most of the pumping. In left-sided heart failure, the left ventricle can't pump as much blood. The extra blood pools in the pulmonary veins—blood vessels that carry blood away from the lungs.
Doctors divide left-sided heart failure into two types based on the heart's pumping ability:
Systolic heart failure happens when the heart muscle doesn't contract with enough force to pump enough blood out to the body. Another name for this is heart failure with reduced ejection fraction (EF). EF measures how well your heart pumps with each beat.
Diastolic heart failure is when the heart contracts normally, but the ventricles don't relax properly or are too stiff. Less blood can fill the heart. Another name for this is heart failure with preserved EF.
Your doctor can tell you which of these conditions you have.
Heart Failure Diagnosis
Your doctor will ask questions like these about your medical history:
- Do you have any conditions that can cause heart failure, such as CAD, diabetes, heart valve disease, or high blood pressure?
- Do you smoke?
- Do you use any drugs?
- Do you drink alcohol, and if so, how much?
- Which medications do you take?
Your doctor will also ask about your symptoms and do a physical exam. They will listen to your heart and look for signs of heart failure. And they will check for other illnesses that may have made your heart muscle weak or stiff.
Your doctor may also order tests like these to find the cause of your heart failure and to see how severe it is:
- Blood tests. You may have tests to see how well your kidneys and thyroid gland work. Other blood tests check for high cholesterol levels and anemia—too few of the healthy red blood cells that transport oxygen through your body.
- B-type natriuretic peptide (BNP) blood test. BNP is a hormone your heart releases. High BNP blood levels can mean your heart doesn't pump as well as it should.
- Chest X-ray. A chest X-ray shows the size of your heart and whether there is fluid buildup around the heart and lungs.
- Echocardiogram. This is an ultrasound that shows the heart's movement, structure, and function.
- EKG or ECG. An EKG records the electrical impulses that travel through your heart.
- Cardiac catheterization. This procedure shows your doctor how well your heart works and whether CAD caused your congestive heart failure.
- Stress test. This test shows how well your heart pumps while you exercise and if there are problems with blood flow. It can help your doctor diagnose coronary heart disease.
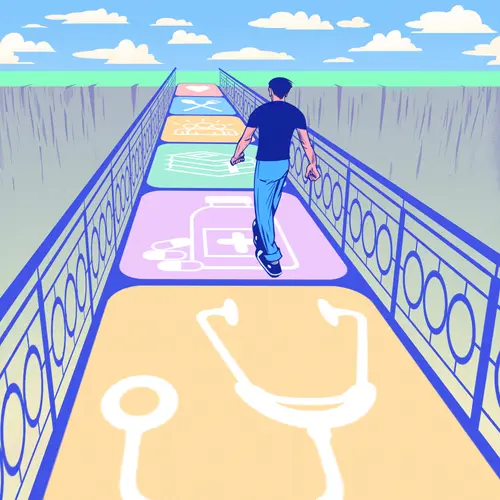
Heart Failure Treatment
There are more treatment options available for heart failure than ever before. Lifestyle changes, medication, and careful monitoring are the first steps. If the condition gets worse, you may need to see a doctor who specializes in treating heart failure.
The goals of heart failure treatment are to prevent it from getting worse, relieve symptoms, and improve your quality of life.
Your doctor might first recommend lifestyle changes like these for early-stage heart failure:
- Weight loss
- Exercise
- A healthy, low-sodium diet
- Smoking cessation
- Stress management
- Enough sleep
Some common types of medicines used to treat heart failure are:
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers to relax blood vessels
- Beta blockers to slow the heart rate
- Angiotensin receptor-neprilysin inhibitors to open up arteries and improve blood flow
- Digoxin to strengthen the heartbeat and help it pump more blood
- Diuretics and aldosterone antagonists to get rid of extra fluid in the body
- Hydralazine or isosorbide dinitrate to widen blood vessels
- Potassium to control the heart rhythm
- Sodium-glucose cotransporter-2 inhibitors to lower blood sugar and blood pressure
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. This program usually includes workouts that are designed just for you, along with advice to help you quit smoking and change your diet.
Cardiac rehab also offers emotional support. You'll meet other people with heart failure who can help you stay on track.
If those treatments don't work, you may need one of these procedures:
Coronary bypass surgery to route blood around a blocked artery.
Heart valve repair or replacement to fix or repair a damaged valve in your heart.
Implantable cardioverter defibrillator to put your heart back into a normal rhythm if it goes out of rhythm.
Cardiac resynchronization therapy, also called a biventricular pacemaker, to help your two lower heart chambers pump blood at the same time.
Ventricular assist device to pump in place of your heart until you can have surgery to fix the problem.
A heart transplant is an option for people with very severe heart failure who haven't improved with surgery or medicine. The surgeon replaces your damaged heart with a healthy heart from a donor.
Can heart failure be reversed?
That depends on the cause. Doctors consider heart failure reversed when the EF goes back to normal.
Some of the conditions that cause heart failure improve on their own, such as:
- Infections like myocarditis
- Cardiomyopathy that's caused by stress
You may be able to bring the EF to normal if you:
- Take medicine to control an irregular heart rhythm or lower blood pressure
- Have a procedure to open blocked coronary arteries
- Stop drinking alcohol or taking drugs that caused heart failure
- Treat a heart valve problem
The longer you've had heart failure and the more damage there is to your heart, the harder it is to reverse. A heart transplant may be the only way to reverse severe heart failure.
Stages of Heart Failure
Heart failure often progresses or gets worse over time.
The American Heart Association and American College of Cardiology divide heart failure into four stages, based on how severe it is. Your doctor will recommend treatments for your stage of heart failure.
In the early stages, lifestyle changes like diet and exercise plus medication may be enough to treat heart failure. Later stages may need surgery or a heart transplant to correct.
Stage A. You're at a risk of heart failure because of a condition like high blood pressure, diabetes, or blood vessel disease. But you don't have any symptoms or problems with your heart.
Stage B. You don't have symptoms, but you do have raised pressure in your heart or problems with your heart's structure.
Stage C. You have or have had symptoms of heart failure.
Stage D. Your heart failure symptoms are severe enough to get in the way of your daily life or put you in the hospital.
The New York Heart Association divides heart failure into four categories based on how much it affects your activity level:
Class 1. Heart failure doesn't affect your activity.
Class 2. Heart failure slightly limits your activity. You have symptoms like tiredness, shortness of breath, heart palpitations, or chest pain when you do daily activities.
Class 3. Heart failure noticeably limits your activities. Even mild activity causes tiredness, shortness of breath, heart palpitations, or chest pain.
Class 4. You have heart failure symptoms even when you're at rest.
How Can I Prevent Heart Failure From Getting Worse?
Follow these tips to protect your heart and slow heart failure:
Treat high blood pressure. In heart failure, blood vessels narrow. Your heart must work harder to pump blood through those narrowed vessels. It's important to keep your blood pressure controlled so that your heart can pump more effectively without extra stress.
Monitor your symptoms. Weigh yourself every day and check your body for swelling. These are signs that you're holding onto fluid. Call your doctor if you gain 3 pounds in 1 day or 5 pounds in 1 week or if you notice any swelling.
Keep a balance of fluids. Your doctor may ask you to write down how much fluid you drink and how often you go to the bathroom. The more fluid you carry in your blood vessels, the harder your heart must work to pump the extra fluid through your body. You may need to reduce the amount of fluid you drink to lower your heart's workload and prevent heart failure symptoms.
Limit salt (sodium). Sodium is naturally in some foods and added to others for flavor or to make food last longer. If you follow a low-sodium diet, you should retain less fluid, have less swelling, and breathe more easily.
Be aware of new or worsening symptoms. Call your doctor if you have new symptoms or if the symptoms you had get worse.
Take your medications as prescribed. Medicines improve your heart's ability to pump blood, lower stress on your heart, slow heart failure, and prevent your body from holding onto fluid. Heart failure drugs help your blood vessels widen and relax, which lowers blood pressure.
Schedule regular doctor appointments. During follow-up visits, your doctors will make sure that you stay healthy and your heart failure doesn't get worse. They will go over your weight and list of medications. If you have questions, write them down and bring them to your appointment. Call your doctor with any urgent questions between visits. Notify all your doctors about your heart failure, medications, and any restrictions. Also, check with your heart doctor about any new medications prescribed by another doctor. Keep good records and bring them with you to each doctor visit.
How Can I Prevent Further Heart Damage?
In an effort to prevent further heart damage:
- Stop smoking or chewing tobacco.
- Reach and maintain your healthy weight.
- Control high blood pressure, cholesterol levels, and diabetes.
- Exercise regularly.
- Don't drink alcohol.
- Have surgery or other procedures to treat your heart failure as recommended.
How can I prevent further damage to my kidneys?
Heart failure raises your risk of chronic kidney disease. Your damaged heart sends less blood to your kidneys. Without oxygen-rich blood, your kidneys can't filter your blood as well. Heart failure and kidney disease also share risks like diabetes and high blood pressure.
These are some ways to protect your kidneys:
- Manage heart failure. Follow the treatment plan your doctor recommends.
- Eat right and exercise. Limit the salt, fat, and sugar in your diet. Try to get at least 30 minutes of exercise each day.
- Lose weight if you are overweight. Excess weight raises the risk of high blood pressure and diabetes, which can harm both your kidneys and heart.
- Lower your blood pressure and blood sugar. Keep your blood pressure below 140/90 or the number your doctor recommends. High blood pressure damages the heart and kidneys. Also, follow your doctor's advice to treat diabetes. High blood sugar damages blood vessels in your kidneys.
What Medications Should I Avoid if I Have Heart Failure?
A few medications can cause problems for people with heart failure, including:
- Nonsteroidal anti-inflammatory drugs such as ibuprofen (Motrin or Advil) and naproxen (Aleve)
- Some drugs that control the heart rhythm
- Calcium channel blockers (if you have systolic heart failure)
- Some nutritional supplements, such as salt substitutes
- Antacids that contain sodium
- Cough and cold medicines that contain pseudoephedrine, such as Sudafed
If you take any of these drugs, discuss them with your doctor.
It's important to know the names of your medications, what they're used for, and how often and at what times you take them. Keep a list of all your medications and bring them with you to each of your doctor visits.
Don't stop any heart failure medication without first talking to your doctor. Even if you have no symptoms, your medications lower your heart's workload so that it can pump better.
How Can I Improve My Quality of Life With Heart Failure?
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also lower heart failure progression.
- Don't overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling, may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
Heart failure diet
A few changes in your diet can reduce the workload on your heart and help improve your symptoms.
- Eat lots of fresh fruits and vegetables.
- Limit salt to less than 1,500 milligrams (1.5 grams) each day. Choose foods that are naturally low in salt, like fish and chicken, fresh beans and peas, eggs, milk, and plain rice.
- Season foods with herbs, spices, and citrus instead of salt.
- Eat foods that are high in fiber, such as oatmeal, almonds, and avocado.
- Cut back on cholesterol, sugar, and trans fats.
Can Surgery Be Used to Treat Heart Failure?
In heart failure, surgery may sometimes prevent further damage to the heart and improve the heart's function. Procedures used include:
- Coronary artery bypass grafting surgery. The most common surgery for heart failure caused by CAD is bypass surgery. Although surgery is more risky for people with heart failure, new strategies before, during, and after surgery have reduced the risks and improved outcomes.
- Heart valve surgery. Diseased heart valves can be treated both surgically (traditional heart valve surgery) and nonsurgically (balloon valvuloplasty).
- Implantable left ventricular assist device (LVAD). The LVAD is known as the "bridge to transplantation" for patients who haven't responded to other treatments and are hospitalized with severe systolic heart failure. This device helps your heart pump blood throughout your body. It allows you to be mobile, sometimes returning home to await a heart transplant. It may also be used as destination therapy for long-term support in patients who are not eligible for transplant.
- Heart transplant. A heart transplant is considered when heart failure is so severe that it doesn't respond to all other therapies, but the person's health is otherwise good.
Heart Failure Treatment Is a Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members—including nurses, dietitians, pharmacists, exercise specialists, and social workers—will help you achieve success.
If you notice anything unusual, don't wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain (more than 2 pounds in a day or 5 pounds in a week)
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate (above 100 beats per minute or a rate noted by your doctor)
- New irregular heartbeat
- Chest pain or discomfort during activity that gets better if you rest
- Trouble breathing during regular activities or at rest
- Changes in how you sleep, like having a hard time sleeping or feeling the need to sleep a lot more than usual
- Less of a need to pee
- Restlessness, confusion
- Constant dizziness or lightheadedness
When Should I Get Emergency Care?
Go to the ER or call 911 if you have:
- New, unexplained, and severe chest pain that comes with shortness of breath, sweating, nausea, or weakness
- Fast heart rate (more than 120-150 beats per minute or a rate noted by your doctor), especially if you are short of breath
- Shortness of breath that doesn't get better if you rest
- Sudden weakness or you can't move your arms or legs
- Sudden, severe headache
- Fainting spells
What Is the Outlook for People With Heart Failure?
With the right care, heart failure may not stop you from doing the things you enjoy. Your prognosis or outlook for the future will depend on how well your heart muscle is functioning, your symptoms, and how well you respond to and follow your treatment plan.
Everyone with a long-term illness such as heart failure should discuss their desires for extended medical care with their doctor and family. An advance directive or living will is one way to let everyone know your wishes. A living will expresses your desires about the use of medical treatments to prolong your life. This document is prepared while you are fully competent in case you are unable to make these decisions at a later time.
Takeaways
About one-quarter of Americans will develop heart failure in their lifetime. Conditions like high blood pressure, diabetes, and CAD raise the risk. If your doctor has diagnosed you with heart failure, make sure you are on a treatment plan and that you follow your doctor's advice to protect your heart from further damage.
Heart Failure FAQs
- How long can a person live with congestive heart failure?
Around half of people with congestive heart failure live for at least 5 years. How long you live depends on how severe your heart failure is and how you treat it.