If your doctor thinks you have heart disease, they will first ask about your symptoms and your medical history. They’ll also give you a medical exam.
Listening to the heart for swishing or whooshing sounds, known as heart murmurs, may give important clues about heart trouble. If they suspect heart disease, they’ll do more tests.
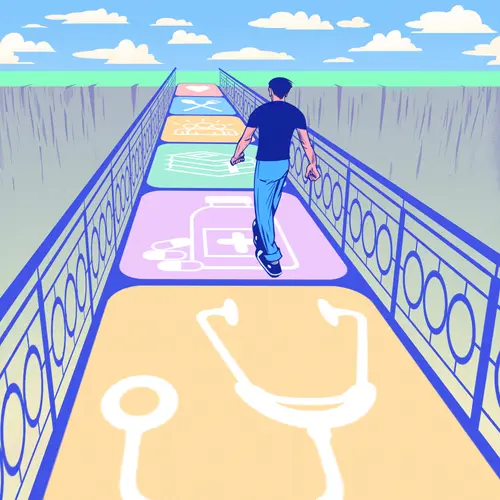
How Is Heart Disease Diagnosed?
An electrocardiogram (EKG) is usually the first test. By recording electrical activity within the heart, the EKG reveals any electrical problems that may be a source of trouble or may show that your heart muscle has been injured by lack of oxygen.
Your doctor might use other tests to diagnose your heart disease, such as:
- Cardiac catheterization
- X-rays
- Scans using CT, MRI, or nuclear technology
- Angiography, a special technique that allows for detailed imaging of blood vessels
- Echocardiograms (ultrasounds of the heart) to find out how well your heart and valves are working
- Stress tests
- Sophisticated testing for arrhythmias, such as electrophysiology or EP testing
- Coronary artery calcium score
- Myocardial biopsy
If you’ve been diagnosed with heart disease, ask your doctor these questions at your next visit.
- What caused my heart problem?
- How severe is my heart problem?
- What treatments do I need, and are there side effects?
- Should I start a cardiac rehab program to make my heart stronger?
- What should I do if my symptoms get worse quickly?
- What can I do to prevent this from getting worse or having a heart problem again?
- Should I eat different foods?
- How will this affect my activities, such as having sex, working, or caring for my children or grandchildren?
- What can I do to feel less stress and worry?
- How often do I need to come in for an office visit?
Heart Disease Types: Symptoms and Treatment
Heart disease has many different types. Each has its own symptoms and treatments, although there is some overlap. With some forms of heart disease, you may not notice any symptoms.
Coronary artery disease
The symptoms of coronary artery disease include:
- Angina, a discomfort, heaviness, pressure, aching, burning, fullness, squeezing, or painful feeling in your chest; it may happen with exertion. It can be mistaken for indigestion or heartburn. Angina is usually felt in the chest, but may also be felt in the shoulder, arms, neck, throat, jaw, or back.
- Shortness of breath
- Palpitations (irregular heartbeats, skipped beats, or a "flip-flop" feeling in your chest)
- Rapid heartbeat
- Weakness or dizziness
- Nausea
- Sweating
- Usually short-lived
- Generally stops with rest
Your doctor may prescribe:
- Daily aspirin
- Drugs such as ACE inhibitors and beta-blockers
- Drugs that treat angina like nitroglycerin or ranolazine
- Medications that target high blood pressure and high cholesterol, two major risk factors for coronary disease
Your doctor also may recommend invasive treatments such as:
- Balloon angioplasty (usually using a stent to prop open the vessels)
- Open-heart surgery to bypass blocked heart arteries
Heart attack
Symptoms of a heart attack include:
- Discomfort, pressure, heaviness, or pain in the chest or left arm
- Fullness, indigestion, or a choking feeling (may feel like heartburn)
- Discomfort radiating to the back, jaw, throat, or arm
- Sweating, nausea, vomiting, or dizziness
- Extreme weakness, anxiety, or shortness of breath
- Rapid or irregular heartbeats
Heart attack symptoms usually last 30 minutes or longer and are not relieved by rest or by taking a heart medication called nitroglycerin. But some people have a heart attack without having any symptoms. A ''silent'' heart attack can happen in anyone, though it happens more often among people with diabetes.
If you think you are having a heart attack, DO NOT DELAY. Call 911. Quick treatment of a heart attack is very important to lessen the amount of damage to your heart.
Heart failure
Symptoms of heart failure include:
- Shortness of breath (often causes a hacking cough)
- Quick weight gain (a weight gain of 2 or 3 pounds in a day is possible)
- Swelling in ankles, legs, and abdomen
- Dizziness
- Fatigue and weakness
- Rapid or irregular heartbeats
- Other symptoms include nausea, palpitations, chest pain, waking suddenly at night unable to breathe, and changes in sleep patterns
- Late symptoms include weight loss and loss of appetite
Heart failure symptoms may not be related to how weak your heart is. You may have many symptoms, but your heart function may be only mildly weakened.
Treatment usually depends on the cause of heart failure but often includes drugs to control symptoms, such as:
- Diuretics or water pills to flush the body of fluids
- Beta-blockers to block adrenaline’s action
- ACE inhibitors to help modulate sodium
Devices such as pacemakers and defibrillators are sometimes implanted to improve the heart's function and prevent deadly arrhythmias. In very advanced cases, heart transplantation may be a consideration.
Arrhythmias
Arrhythmia symptoms include:
- Palpitations (a feeling of skipped heartbeats, fluttering, or "flip-flops," or feeling that your heart is "running away")
- Pounding in your chest
- Dizziness, feeling lightheaded or fainting
- Shortness of breath
- Chest discomfort
- Weakness or fatigue
Treatment depends on the type of arrhythmia you have but can include:
- Drugs to lower the heart rate
- Drugs to convert your rhythm to normal
- Drugs to prevent blood clots
- Cardioversion, a treatment that involves sending a strong electrical shock to your heart to convert its heart rhythm back to normal
Heart valve disease
Symptoms of heart valve disease include:
- Shortness of breath or trouble catching your breath
- Weakness or dizziness
- Fainting
- Discomfort in your chest during an activity
- Palpitations that may feel like a rapid heart rhythm, irregular heartbeat, skipped beats, or a flip-flop feeling in your chest
If valve disease causes heart failure, symptoms include:
- Swelling of your ankles, feet, or abdomen
- Quick weight gain (a weight gain of 2 or 3 pounds in one day is possible)
Symptoms do not always relate to the seriousness of your valve disease. You may have no symptoms and have severe valve disease, or you may have severe symptoms but minor valve disease. Often, the first sign of valve problems is a heart murmur that is found during a routine physical exam.
If your heart valve disease is severe, you may need treatment with medications to deal with heart failure. You also may need invasive procedures to repair or replace the valve.
Congenital heart disease
In adults, symptoms of congenital heart disease include:
- Shortness of breath
- Limited ability to exercise
- Symptoms of heart failure or valve disease
Symptoms of congenital heart disease in infants and children include:
- Bluish tint to the skin, fingernails, and lips
- Fast breathing and poor feeding
- Poor weight gain
- Frequent lung infections
- Inability to exercise
Some minor conditions can clear up on their own or can be treated easily with medications. Those that are more complex can often be treated surgically, if necessary. Very rarely, the heart problem is so severe that it cannot be corrected.
Heart muscle disease (cardiomyopathy)
Many people with heart muscle disease have no symptoms or only minor symptoms and live a regular life. Other people have symptoms that get worse as heart function worsens.
Symptoms of cardiomyopathy can happen at any age and may include:
- Chest pain or pressure (usually with exercise or physical activity but can also happen with rest or after meals)
- Heart failure symptoms
- Swelling of the lower extremities
- Fatigue
- Fainting
- Palpitations (fluttering in the chest due to uneven heart rhythms)
Sudden death can happen in a small number of people with cardiomyopathy.
Treatment for cardiomyopathy will depend on the cause but often includes the same measures used for patients with heart failure. The outcome is also dependent upon the underlying cause. In some cases, heart transplant surgery may be recommended.
Pericarditis
Symptoms of pericarditis include:
- Chest pain. This is different from angina. It may be sharp and located in the center of the chest. The pain may radiate to the neck and occasionally, the arms and back. It’s worse when you lie down, cough, swallow, or take a deep breath, and it’s better when you sit forward.
- Low-grade fever
- Increased heart rate
Pericarditis often eases on its own, but it also can be treated with:
- Anti-inflammatory drugs such as aspirin
- In severe cases, steroids
Sometimes, fluid must be drained from the pericardium using a long, thin needle inserted carefully through the chest. If a chronic condition develops, a pericardial window may need to be created surgically to let this fluid drain.
Rarely, surgery may be needed to make a pathway for the extra fluid to drain internally or remove the pericardial sac completely.
Dietary Supplements for Heart Disease
Researchers are looking at several dietary supplements to find out if they treat heart disease. They include L-carnitine, coenzyme Q10, and garlic. So far, these are not recommended for treating or preventing heart disease.
Vitamins E and C have been studied thoroughly and do not appear to lower the risk of developing heart disease. In general, you’ll get the most benefits from vitamins and other micronutrients when you get them from whole foods.
Stay on Track
With heart disease, it may feel like you're going through a lot of changes all at once. It's a good idea to get help from dietitians, doctors, and support groups to keep focused.
Some of the keys to making changes are:
- Have a plan before starting.
- Set realistic targets.
- Make one change at a time. For example, quit smoking before you overhaul your diet.
- Write down your goal.
- Prepare for setbacks. They happen. What matters more is that you get back on track.
- Reward yourself for your progress. Pick a treat that feels great but doesn't undermine your game plan.
- Keep up with your friends and family. Your social connections are good for you.
Also, stay in touch with your mood. For many folks, depression comes along with heart disease. If you notice that's true for you, talk to your doctor to get treatment.
When to Call Your Doctor
Call your doctor if:
- You have unusual chest pain, especially if it doesn’t go away or if it comes back. It could be heartburn, but it could also be a sign of angina or a heart attack.
- You have recurring disturbances of your heartbeat. If frequent or persistent, uneven heartbeats may signal a serious heart condition.
- You become suddenly dizzy, lightheaded, weak, or faint. Even if the cause is not heart disease, it could be serious.