What Is a Ventilator?
A ventilator, sometimes called a mechanical ventilator, is a machine that helps you breathe when you're sick, injured, or sedated for an operation. It pumps oxygen-rich air into your lungs. It also helps you breathe out carbon dioxide, a harmful waste gas your body needs to get rid of.
Even while they help you breathe, ventilators sometimes lead to complications. These problems can result from the ventilator itself, or from things that are more likely to happen when you're on a ventilator.
Ventilator vs. respirator
People sometimes use the word respirator to mean the same thing as ventilator. The CDC defines a respirator as a mask or device that protects you from dangerous particles in the air. But a respirator can also describe a device that helps you breathe, like a ventilator.
Ventilator vs. intubation
Ventilators and intubation are often used together, but they aren't the same. Intubation is a procedure in which a health-care worker places a tube down your throat to move air in and out of your lungs. This tube can then be hooked up to a bag or a ventilator machine.
Types of Ventilators
There are several types of ventilation. Your doctor will determine which is best for your situation.
Noninvasive ventilation
Noninvasive ventilation involves using a face mask that connects to the ventilator. You breathe into the mask, which straps around your head. Two common noninvasive ventilation devices are continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP) machines, both used by people with sleep apnea.
Invasive ventilation
With invasive ventilation, you have a tube in your airway that connects to a ventilator machine. The tube can either enter through your mouth (intubation) or through an incision a doctor cuts into your neck (tracheostomy).
Mechanical ventilator
A mechanical ventilator is a machine that keeps your airways open and delivers oxygen to help you breathe. It's considered a form of life support.
Face mask ventilator
A face mask ventilator is a form of noninvasive ventilation. It essentially means you wear a face mask to get oxygen. It may be used to deliver anesthesia as well as to help you breathe.
Manual resuscitator bag
A manual resuscitator bag provides air by hand. Someone pumps the bag to help air go in and out of your lungs. The bag can attach to a face mask ventilator or a tube if you're intubated. This may be an option if a mechanical ventilator isn't available or stops working.
Tracheostomy ventilator
With a tracheostomy ventilator, the machine attaches to a tube that doctors have inserted into an opening in your neck.
Ventilator Uses
There are several reasons you might need to use a ventilator, either for a short time or long term.
Ventilator for surgery
General anesthesia (the kind that makes you sleep) can make it hard to breathe on your own. A ventilator can help until the anesthesia wears off.
Ventilator for respiratory failure
When you have a hard time breathing on your own, that's called respiratory failure. it can happen suddenly, due to something like a drug overdose or an injury to your lungs or spinal cord. Or it can be long-lasting (chronic) when you have a health condition that affects your breathing, such as:
Brain injury or stroke
You may need a ventilator when damage prevents your brain from telling your lungs to breathe properly.
Other health conditions
Many other health conditions may require ventilation, including:
- Coma
- Pneumonia
- Chronic obstructive pulmonary disease or COPD, a chronic inflammatory lung condition
- Acute respiratory distress syndrome or ARDS, a lung injury that lets fluid leak into the lungs
- Anaphylaxis, a serious allergic reaction
- Certain diseases that affect the nerves and muscles
Ventilator for COVID-19
The virus that causes COVID-19 can cause respiratory failure. In serious cases, it can inflame your airways and essentially drown your lungs in fluids. A ventilator can help you breathe while your body fights the virus.
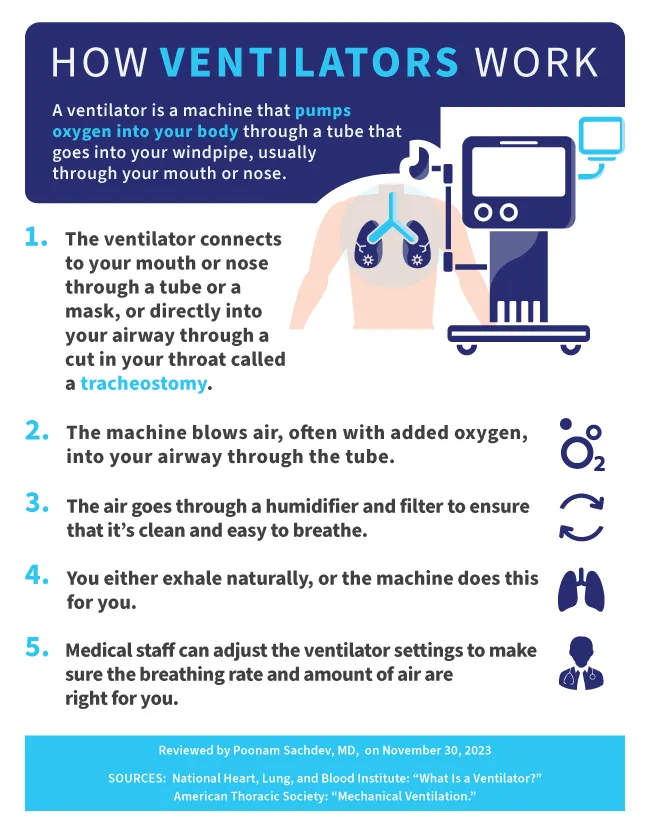
How Does a Ventilator Work?
A ventilator connects to a face mask or to a tube in your nose, mouth, or throat. It blows oxygen-rich air into your windpipe through the tube. Before it travels to your windpipe, the air passes through a humidifier, which keeps it warm and moist. The ventilator may also breathe out for you, or you may do it on your own.
The machine maintains a constant low pressure to prevent the air sacs in your lungs from collapsing.
The ventilator can be set to take a certain number of breaths for you per minute. Your doctor also may program it to kick in when you need help. In this case, the machine will blow air into your lungs automatically if you haven't taken a breath in a set amount of time.
What to Expect on a Ventilator
When you're on a ventilator, you might feel discomfort. But it won't hurt. Your doctor will give you medicines to keep you relaxed. Often, people on ventilators are awake, but they may not be fully aware of what's going on. If your condition is serious, your doctor might keep you asleep, so your body can heal better.
Your health team will monitor you often. They may check your blood pressure, heart rate, oxygen levels, and breaths per minute. You might also have chest X-rays and blood tests during ventilation. A respiratory therapist will probably suction your breathing tube to help clear mucus from your lungs.
If you have a face mask, you may be able to take it off temporarily to eat or talk. You won't be able to talk or eat or drink normally if you're intubated. In this case, you'll get fluids from an IV and nutrition through a tube in your stomach.
Your doctor will have you sit up often or lie on your stomach to help your lungs get more oxygen. In some cases, you may even walk around while on a ventilator.
Ventilation can be upsetting for both the person getting it and their loved ones. If someone you know is on a ventilator, here are some ways you can help:
- Stay positive. When you see someone on a ventilator, you may feel upset or emotional. Try to remain upbeat.
- Help them find ways to communicate. You can use gestures or write words down.
- Talk to them often.
- Touch or hold their hand.
- Bring them familiar items. A pillowcase or robe from home might make them feel more comfortable.
Ventilator Complications
Even while they help you breathe, ventilators sometimes lead to complications. These problems can result from the ventilator itself, or from things that are more likely to happen when you're on a ventilator.
Infection
The breathing tube in your airway could let in bacteria that infect the tiny air sacs in the walls of your lungs. Plus, the tube makes it harder to cough away debris that could irritate your lungs and cause an infection.
This type of infection is called ventilator-associated pneumonia, or VAP. It's especially risky because you may already be quite sick when you're put on a ventilator. VAP can make it harder to treat your other illness.
Doctors treat it with antibiotics. In some cases, VAP might require special types that can fight antibiotic-resistant bacteria.
Even if you already have an infection, like a viral infection of your lungs, you can get VAP on top of that. Doctors call this a "superinfection."
Lung damage
Medical staff members carefully measure the amount, type, speed, and force of the air the ventilator pushes into and pulls out of your lungs. Too much oxygen in the mix for too long can be bad for your lungs. If the force or amount of air is too much, or if your lungs are too weak, it can damage your lung tissue. Your doctor might call this ventilator-associated lung injury (VALI).
Among the conditions VALI can lead to are:
- Pneumothorax: A hole or holes in your lungs that release air into the opening between your lungs and the wall of your chest. This can cause pain and loss of oxygen. It might also cause your lungs to collapse, which is an emergency.
- Pulmonary edema: The buildup of liquid in your lungs. Your lungs may collect more liquid if you already have pneumonia.
- Hypoxemia: Too little oxygen in your blood. Damage to your lungs can cause this. Medical staff will notice it if your blood oxygen levels start to drop and you are short of breath.
Other risks
Other issues that can happen due to ventilator use include:
- Delirium: You're usually unconscious or heavily sedated when you're on a ventilator. Either way, you take strong medications. Sometimes, these drugs may take some time to wear off even after the tube is removed from your airway. You may have a hard time reading, writing, or thinking clearly. You also might notice a poor memory, have trouble sleeping, feel anxious, or have unusual emotions like paranoia. Talk to your doctor about these effects, which should fade over time.
- Immobility: You can't move much when you're on a ventilator, especially when you're sedated. That can lead to bedsores, which may turn into skin infections. You're more likely to get blood clots for the same reason. Your muscles, including those that normally help you breathe for yourself, may get weak. You might need rehab with a physical or respiratory therapist.
- Vocal cord problems: When your doctor removes the breathing tube to take you off the ventilator, it can damage your vocal cords. Expect some soreness and a raspy voice at first. But let your doctor know if it's hard to breathe or speak after the tube comes out.
Signs of death while on a ventilator
When someone dies while on a ventilator, the machine will keep breathing for them. When the lungs have oxygen, the heart can still beat, and their skin can still be warm. But they won't breathe if the ventilator is turned off, because they have no brain activity (brain death). Other signs of brain death include:
- No reaction to pain or touch
- Eyes don't move or blink
- Pupils don't respond to light
- No gag reflex
An electroencephalogram (EEG) can detect whether a person has any brain activity.
Using a Ventilator at Home
Most often, ventilators are used in health care settings like hospitals and ambulances. But your doctor may suggest that you use one at home if you need the machine long-term or if your condition is stable.
A health care professional will show you how to properly use the device. You'll need to be able to recognize if there's a problem with the machine. And you should know what to do in case of an emergency.
The type of ventilator you take home may depend on your medical condition. Some are more portable than others.
The equipment and supplies you may need for your ventilator are:
- A backup ventilator and extra oxygen tank for emergencies
- Batteries
- A humidifier to add moisture to the air
- A suction machine to remove mucus
- A pulse oximeter, which checks your blood oxygen levels
- A nebulizer, which is a machine that delivers medicines to help you breathe better
Weaning Off a Ventilator
When you can breathe on your own, your doctor will remove your tube and take you off the ventilator. At first, you may require other devices, such as ventilation with a mask or an oxygen mask, to help you breathe. Sometimes, you may need to be put back on a mechanical ventilator if you aren't breathing well on your own.
When the tube is removed, you may have a sore throat, an irritated mouth, or hoarseness. Some people also notice brain fog, problems with thinking, and physical weakness after coming off a ventilator.
Recovery times vary, but some experts say you'll need at least a week for every day that you were on the ventilator. That means if you were on a ventilator for three days, it will likely take three weeks before you feel normal again.
