Slideshow: OAB -- Helping a Confused Bladder


What is Overactive Bladder?
How often do you usually use the bathroom daily? Is it more than seven or eight times -- and you can't wait? Are you getting up more than once or twice a night to go? Do your trips to the bathroom cause problems with your job, social life, or relationships? You may have an overactive bladder. At least 33 million Americans have OAB.
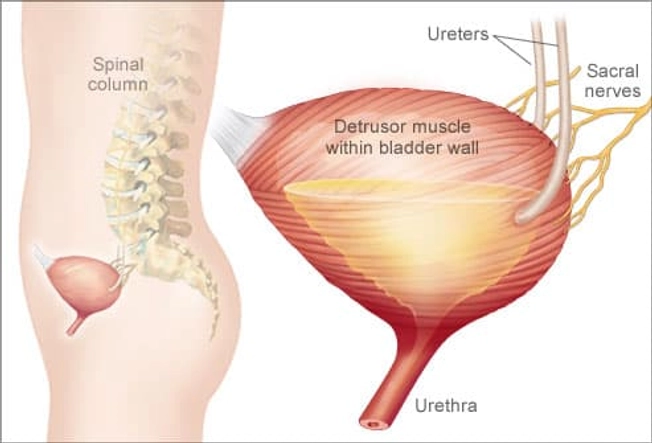
How the Bladder Gets Confused
Your body keeps urine in the bladder. When it's full, nerves tell the muscles around your bladder it's time to push urine out. Other nerves tell the urethra -- the tube from the bladder -- to open so urine can leave your body. Sometimes nerve signals can get mixed up, telling your bladder it's time to go, even when it isn't full. That's OAB.

OAB vs. Incontinence
About two-thirds of women with OAB are "OAB dry." They feel like they have to go right away -- and go often -- but they can make it to the bathroom in time. Others are "OAB wet." They often have accidents along with their OAB. This is usually urge incontinence, which is leaking after a sudden, strong need to urinate.

What Causes Signal Problems?
Sometimes the cause of OAB is simple and easy to treat, such as a urinary tract infection. Other causes might be nerve damage from injury or pelvic surgery, bladder stones, diabetes, kidney disease, side effects of some drugs, and neurologic disorders like Parkinson's disease, stroke, or multiple sclerosis. But often, the cause of OAB is a mystery.

Diagnosing OAB
These tests can help figure out the cause of your OAB:
- Cystometry: Checks how much urine your bladder can store and your ability to sense fullness, and helps detect nerve overactivity
- Postvoid residual volume: Measures the amount of urine left in your bladder after you empty it
- Urinalysis: Tests the makeup of your urine
- Uroflowmetry: Measures your urine's speed and volume

How Bad Is It?
Your doctor may ask you questions to help figure out how much OAB is affecting your life. For example, you could rate on a scale of 1 to 5 how much you've been bothered by things like accidental leaks, lots of daytime bathroom breaks, and waking up at night to go. Your doctor might also ask you to keep a voiding diary of your bathroom trips.
Lifestyle Treatments
To lessen the effects of OAB, cut down on caffeinated drinks, alcohol, chocolate, tomatoes, citrus, and spicy foods. But don't cut back on your fluids. That could make your urine concentrated, which can irritate your bladder. To prevent constipation, which can also make OAB worse, eat a high-fiber diet. Your doctor may want you to try retraining your bladder through a process of scheduled bathroom breaks.

Pelvic Floor Exercises
Doctors often suggest exercises called Kegels. You can do Kegels anywhere -- in the car, in a meeting, while watching TV -- and no one will know. Just squeeze and hold the muscles you use to stop the flow of urine. Then release, and repeat. Sometimes biofeedback therapy can help teach you which muscles to use and help measure your muscle strength.

Medications for OAB
If lifestyle changes and behavioral treatments don't relieve OAB symptoms, the next step is usually medication. Anticholinergics are the most common OAB medications. You take them by mouth at least once a day. Topical estrogens -- vaginal rings, tablets, or creams -- are also prescribed to treat women's OAB symptoms. Anticholinergics or beta adrenergic agonists (mirabegron, vibegron) are the most common OAB medications.
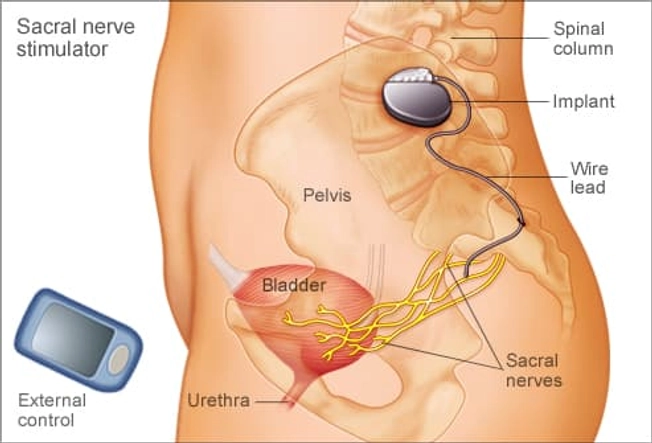
A Stimulator for Your Bladder
When more conservative treatments don't work, a pacemaker-like device can stimulate bladder nerves. It's implanted through a tiny cut above the tailbone during outpatient surgery. Another option, done in the doctor's office, is stimulating the posterior tibial nerve (which is found near the ankle, surprisingly).

Botox for Your OAB
Botox isn't just for your forehead anymore. Doctors inject the drug directly into various places in the bladder muscle. That partially paralyzes it to ease overactivity, but leaves enough control so you can still go. Just as with wrinkles, the Botox effect doesn't last forever.

Another OAB Surgical Option
When nothing else has worked, bladder augmentation uses a patch of your own tissue to make your bladder bigger. But this is considered major surgery, and the procedure is rarely performed. Most people find a combination of lifestyle changes and other treatments that control their OAB.