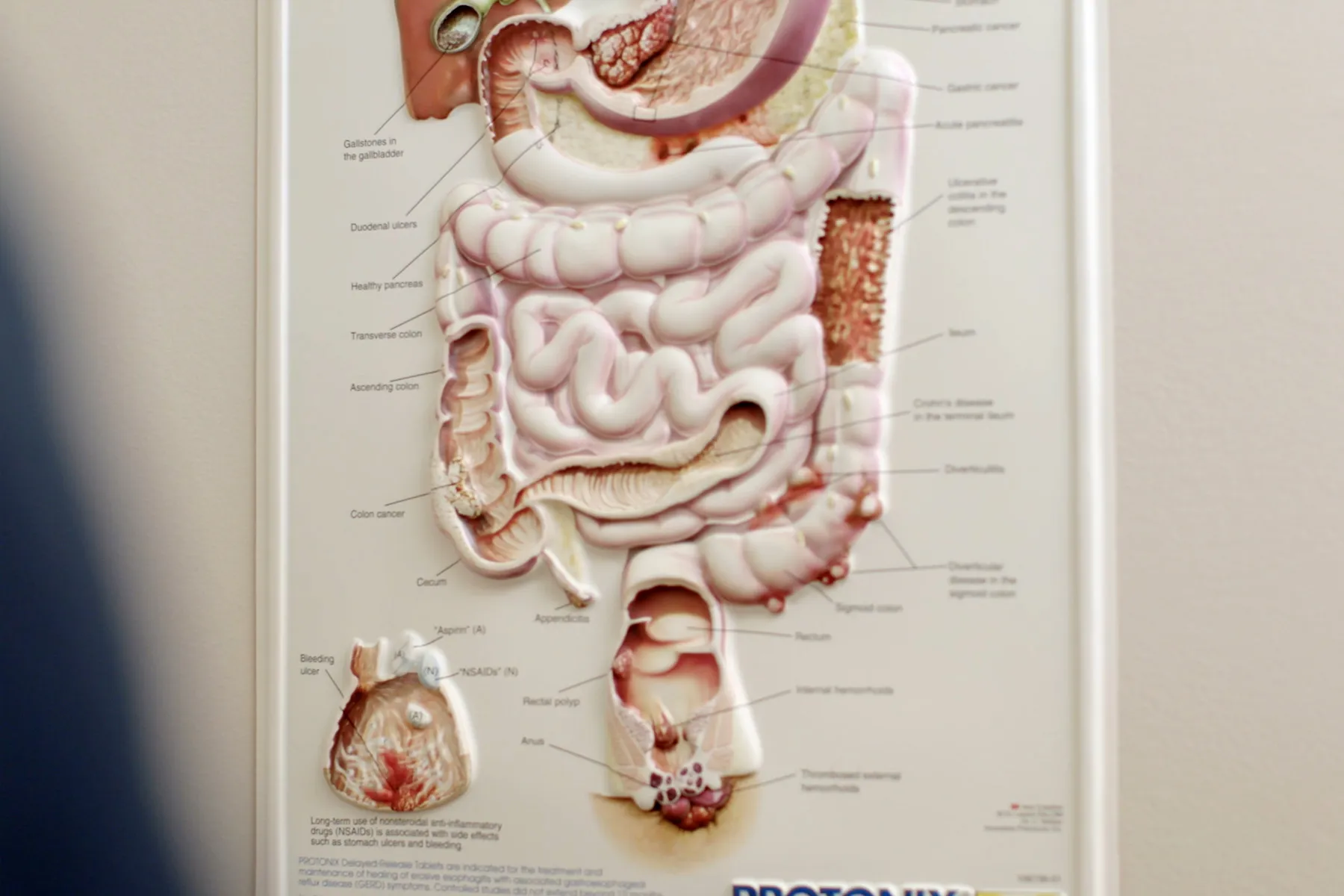
Crohn's disease causes swollen, irritated tissue in your digestive tract. Crohn's can affect any part of it, from the mouth to the anus, but it most often involves the small intestine and colon.
Crohn's and another disease called ulcerative colitis (UC) belong to a group of conditions called inflammatory bowel disease (IBD). Like Crohn's, UC triggers inflammation, but only in the colon.
When you have Crohn's, chances are you'll notice digestive symptoms first. You may have diarrhea, stomach pain, and an urgent need to use the bathroom.
About 40% of those with Crohn's have problems in other areas, such as the joints, eyes, and skin. Digestive symptoms and medications can also lead to these issues.
There's no cure for Crohn's, but treatments can help keep the symptoms in check so you can live a full life.
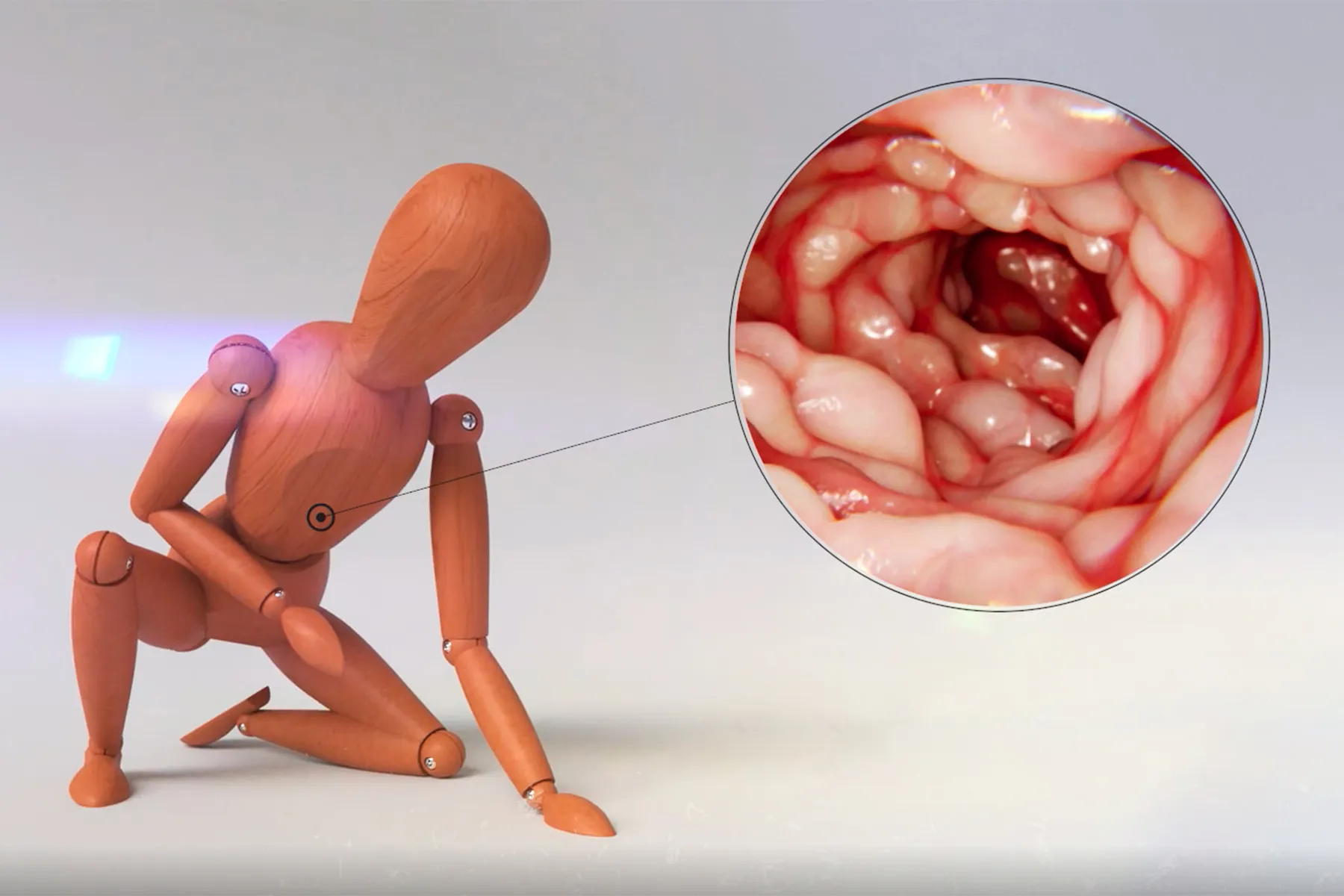
Crohn's starts in the digestive tract. It can show up in patches of healthy or inflamed tissue while not affecting other tissue at all. Often, the inflammation can extend through the entire wall of the intestine.
Symptoms depend on where the disease happens and how serious it is. You can have a period of more severe symptoms -- called a flare -- followed by few or no symptoms, or a remission. About half of Crohn's patients are in remission or have only a mild case in the 5 years after their diagnosis and treatment.
Crohn's can cause these problems in the digestive tract:
Diarrhea
This is one of the most common Crohn's symptoms. When the intestines become inflamed, they can't absorb the same amount of fluids and nutrients. Your stools become loose and watery. You may take more trips to the bathroom.
Ulcers
Chronic inflammation can cause open sores called ulcers. They can happen anywhere along the digestive tract, including the mouth, intestines, and anus. Large ulcers may bleed and cause bloody stools.
Fistulas
Sometimes ulcers can stretch through the wall of the intestine. This creates a tunnel between two organs that don't usually connect, such as the intestine and skin. This is called a fistula. They can cause symptoms such as a painful bump on the skin or urinary tract infections. Up to half of all people with Crohn's will develop a fistula at some point.
Constipation
Although diarrhea is more common, Crohn's can also cause constipation. Inflammation in the lower part of the colon can make it hard to pass stools. Some medicines, such as certain painkillers and iron supplements, could also be the problem.
Cholangitis
Bile ducts carry bile, a digestive fluid, from your liver and gallbladder to the small intestine. In rare cases, Crohn's disease can cause these ducts to become inflamed. That's called cholangitis. It can lead to fever, chills, and pain in the upper right part of your belly.
Gallstones
Having Crohn's may almost double your risk of having gallstones. Those are rock-like deposits of bile. Bile is processed in the small intestine. If Crohn's damages that area, it may not absorb all of the salts in bile. This can lead to a buildup that hardens into gallstones.
Kidney stones
When Crohn's strikes your small intestine, it can't absorb as much fat. These fats bind with calcium, causing hard deposits to form in your kidneys.
Bile duct cancer
Chronic inflammation in your bile ducts may lead to cancer. In fact, Crohn's raises your risk of bile duct cancer by almost threefold. Signs include a yellow tint to your skin and eyes, itchy skin, white stools, and fatigue.
Cirrhosis
Crohn's can lead to inflammation in the liver. About 5% of the time, it develops into a serious liver disease. If the disease isn't treated, it can cause permanent scarring. This is cirrhosis. Cirrhosis can keep your liver from working properly, leading to fatigue; a loss of appetite; swelling in the feet, legs, or ankles; and itchy skin.
As many as 30% of people with IBD have joint problems, too. There are two main forms:
Arthralgia
Joint pain without inflammation
Arthritis
Joint pain with inflammation. Arthritis causes swollen joints and less flexibility.
Arthritis usually affects older people. But it can strike people with Crohn's at a younger age, too.
The main types include:
Peripheral arthritis
This arthritis usually affects the large joints of the arms and legs, such as the knees, wrists, and elbows. The pain can move from one area to another. Most cases don't cause permanent damage.
Axial
arthritis
This is pain and stiffness in the lower spine. Your bones can fuse together and limit your range of motion.
Ankylosing spondylitis
A more severe kind of spinal arthritis, this disease may lead to inflammation in the eyes, lungs, and heart valves.
Having Crohn's ups your chances of heart problems. Research shows that IBD raises the risk of heart disease by about 20% and heart attack by more than twofold.
Although experts are still studying the link, they think these factors are at fault:
Inflammation
People with Crohn's have higher levels of inflammation in their bodies. Chronic inflammation promotes the growth of artery-clogging plaques. When parts of these plaques break off, this can trigger blood clots that cause heart attacks and strokes.
Anemia
One in three people with Crohn's have anemia, a condition where you don't have enough red blood cells to carry oxygen. Your heart has to pump more blood to make up for the lack of oxygen. This can lead to an irregular heartbeat, enlarged heart, or heart failure.
Medications
When taken for a long time, steroids may raise the risk of heart disease and heart failure.
If you have any symptoms of heart disease, such as chest pain or tightness, shortness of breath, and pain or weakness in your arms or legs, see your doctor as soon as possible. These symptoms are often vague, and you may not realize that you have a heart issue until you have a heart attack or stroke.
It's important that you talk about your heart health with your doctor. The goal is to get your inflammation in check. Your chances of having a heart attack or stroke are highest during a flare. If you have anemia, you'll need to treat it. Your doctor may prescribe iron or vitamin B12 supplements.
About 10% of people with IBD, such as Crohn's, have eye problems. Inflammation may affect the eyes, causing them to become red, swollen, and painful. If you have any eye symptoms, talk to your doctor. You may have one of these issues:
Uveitis
This condition is when the middle layer of the eye wall (uvea) becomes inflamed. This causes pain, redness, blurry vision, and light sensitivity. Uveitis is the most common eye issue for people with IBD. Steroid eye drops can ease the inflammation.
Episcleritis
Inflammation of the outer coating of the whites of your eyes (episcleral tissue) can lead to mild redness and soreness. It often clears on its own, but your doctor may prescribe anti-inflammatory eye drops or medicine to treat painful or chronic cases.
Dry eye
Your eyes need vitamin A to make quality tears. If Crohn's is causing low vitamin A levels, you may not produce or keep enough tears in your eyes. This dryness can cause itching, burning, and infection. Artificial tear drops are soothing, and vitamin A supplements can treat the condition.
Keratopathy
In keratopathy, white deposits form on the edge of the cornea. Uveitis and dry eye can set the stage for this condition. Keratopathy doesn't cause pain or affect vision, so it's usually left untreated.
People with Crohn's often deal with skin problems, including sores, bumps, and more.
Common conditions include:
Erythema nodosum
Around 2%-10% of people with IBD have this skin condition. It causes tender, red bumps on the shins or ankles. Sometimes they're on the arms. They often appear during or right before a flare. Your doctor may adjust your medicines to control the underlying inflammation.
Pyoderma gangrenosum
This condition starts with small blisters, most often on the shins and ankles. They can join together to form a large, painful open sore. These sores tend to heal when your Crohn's symptoms are under control. They're treated with antibiotics, shots, and ointments that you rub onto the sores.
Anal fissures
Crohn's can cause small, painful cracks or tears in your anus. Warm baths and ointments can ease the discomfort.
Skin tags
These are small growths of skin. In Crohn's, they often form near the anus. As fissures or swelling heals, the skin can thicken and turn into small flaps. While skin tags are harmless, they can become irritated if moisture or feces become trapped in them. Keeping the area clean can prevent itchiness.
Canker sores
A flare can trigger small mouth ulcers. They usually appear between the gums and lower lip or along the sides or base of the tongue. A medicinal mouthwash can ease the pain.
Rash
Sulfasalazine can lead to an allergy-like rash, while anti-TNF agents (like adalimumab and infliximab) can cause one that looks like psoriasis. It's usually found on the palms, feet, scalp, and behind the ear.
Stretch marks, acne, and thin skin
Taking steroids for a long period of time can lead to skin issues.
Having Crohn's can weaken your skeleton. As many as 60% of people with Crohn's or UC have lower-than-average bone density. Some have thinning bones, or osteoporosis. Others have low bone density, called osteopenia, or softening bones, osteomalacia. All of these conditions may raise your risk of suffering bone breaks and fractures.
It's normal to lose some bone later in life. Your body is constantly clearing old bone tissue and replacing it with new. After around age 35, you start to lose bone faster than you can replace it.
But Crohn's may speed up this process in these ways:
Inflammation
The chemicals that cause inflammation also disrupt your bone turnover. If you get flares often, you're at greater risk for osteoporosis.
Corticosteroids
Taking these anti-inflammatory drugs for a long time can weaken bones. They lower calcium levels and the production of bone-building cells.
Vitamin D deficiency
Your body needs vitamin D to absorb bone-building calcium. Vitamin D is processed in the small intestine, so if Crohn's strikes that area, you may not get enough of the nutrient. This can lead to bone loss.
To protect against bone loss, your doctor may lower your steroid use or prescribe another type of medicine. You may also need to take medication to slow bone loss or stimulate growth.
Crohn's can affect your menstrual cycle. Your periods may come more or less often or not at all. You may also have more cramps and pain when you menstruate.
Experts think that inflammation can shut down normal hormone function. Stress and a lack of nutrition may also throw your menstrual cycle out of whack. Fluctuating hormones can also worsen your Crohn's symptoms.
Fatigue is a common symptom of Crohn's. No matter how much you rest, you still feel exhausted. Crohn's causes this overwhelming sense of tiredness for different reasons:
Inflammation
Chemical signals from inflammation can act on the brain, causing fatigue.
Medication side effects
Certain drugs you take for Crohn's, such as methotrexate and antidepressants, can cause fatigue or sluggishness. Steroids may interrupt sleep.
Nutritional deficiencies
Low levels of iron, B12, and folate are linked with weakness. They can also lead to anemia, which means you have fewer blood cells to carry oxygen to the rest of the body. This can make you tired.
Poor sleep
Symptoms, such as pain and anxiety, can keep you up at night.
When you have Crohn's, it's normal to feel sad or anxious at times. Dealing with the pain and symptoms of the disease is stressful. While these emotions don't cause Crohn's, they can trigger flares and worsen symptoms.
That's why it's important to take care of yourself.
Managing Crohn's means taking care of your body. But it's important to pay attention to your mental health, too. Regular self-care can keep you from feeling too stressed or overwhelmed.
If your emotions get in the way of your life or last for more than a few weeks, see a mental health professional.
It can get worse if it's not addressed. You may need one or both of these treatments to start feeling like yourself again:
Therapy
You'll work with a mental health professional to learn skills for dealing with your condition. You may practice meditation and relaxation. In cognitive behavioral therapy, you'll identify and change thoughts and patterns that lead to depression.
Medications
Your doctor may prescribe an antidepressant or anti-anxiety medication.
There's no single treatment for Crohn's. You'll work closely with your doctor to reduce inflammation and prevent complications. The goal is easing your symptoms and going into long-term remission.
Over the course of your disease, your doctor will probably recommend lifestyle changes, including:
Steer clear of NSAIDs
These painkillers, including aspirin and ibuprofen, may irritate your digestive tract and trigger flares.
Quit smoking
Smoking can set off flares. Quitting the habit can reduce the amount of medicine you need and your risk of needing surgery.
Avoid certain foods
When your Crohn's symptoms are acting up, certain foods can make things worse. They may set off cramps, bloating, and more. These foods often vary from person to person. To discover your triggers, keep a food diary. Your health care team may suggest an elimination diet, where you avoid foods to find out which ones set off symptoms. But there are some common foods that experts recommend avoiding.