A Guide to Metabolic Dysfunction-Associated Steatohepatitis (MASH)
What Is MASH?
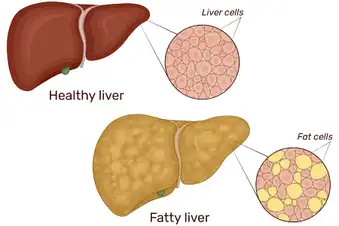
This is a serious form of another condition called metabolic dysfunction-associated steatotic liver disease (MASLD). It used to be called nonalcoholic steatohepatitis (NASH). With MASH, your liver swells from excess fat along with inflammation. MASH can cause cell damage that affects how well your liver works. Over time (usually many years), you may get liver scarring that doesn’t heal. Doctors call this cirrhosis, but it doesn’t happen to everyone.

What Causes MASH?
Doctors can’t say for sure, but people who get this type of liver disease tend to have certain medical conditions in common. Most folks have a higher body weight or type 2 diabetes. Metabolic problems like high cholesterol, high triglycerides, and insulin resistance may also inflame and scar your liver. Certain medications are linked to MASH, including steroids or some drugs that treat cancer or abnormal heart rhythms.

Who Is More Likely to Get MASH?
Anyone can get MASH, even kids. But doctors diagnose it most often in people between the ages of 40 and 60. This type of liver disease typically affects females more than males; it tops the list for why women need a liver transplant. MASH also seems to be more common among people who are Mexican American or Hispanic compared to people of other races and ethnicities.
How Common Is MASH?
Anywhere from 1.5% to 6% of U.S. adults may have MASH. This includes about 20% of everyone with MASLD. But most people with liver disease have a buildup of fat but little to no inflammation or liver cell damage. Some people call this simple fatty liver.
What Are the Symptoms of MASH?
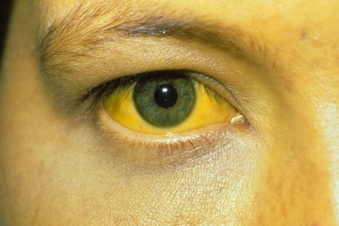
Most people don’t have any. But sometimes MASH can make you tired. Pressure or a mild ache may settle into the upper right part of your belly. If you have serious liver damage, you may start to bleed or bruise easily. You may feel weak. And your skin may itch or turn yellow (called jaundice).

How Is MASH Diagnosed?
Signs of liver damage can show up in routine blood tests, but you’ll need more tests to confirm MASH. That typically includes an ultrasound, CT scan, or MRI. These imaging tests check for fat buildup in your liver. Some hospitals may use a type of ultrasound called a FibroScan or transient elastography. Your doctor may also take tissue from your liver and send it to a lab. A biopsy can pinpoint inflammation and damage caused by MASH.

Can Medication Reverse MASH?
The medication resmetirom (Rezdiffra) has been approved to treat MASH in combination with lifestyle changes aimed at weight loss like diet and exercise. You may also need medication to control high blood sugar or high cholesterol. Some people may benefit from medicine or surgery to help weight loss if lifestyle changes have not been successful. Your doctor might suggest vitamin E, but don’t take any supplement without getting medical approval first. Lifestyle changes can also stop or reverse MASH.

Lifestyle Changes to Manage MASH: Weight Loss
Weight loss can help people with larger bodies improve their liver health. A loss of 3% to 5% of your body weight can cut fat from your liver. To lower inflammation and scarring from MASH, you’ll need to lose at least 7% to 10%. It’s best to shed weight slowly. Around 1 to 2 pounds a week is a good goal. Talk to your doctor about how to lose weight safely. If diet and exercise aren’t enough, ask if surgery or medication are right for you.

Lifestyle Changes to Manage MASH: Exercise
Regular movement can protect against liver damage even if you don’t lose any weight. Aim to get your heart rate up for 150 minutes or more each week. You can garden, take a brisk walk, run, swim, bike, or dance. The key is to find high or low-intensity aerobic exercises you’ll enjoy for 30 to 60 minutes most days of the week. Check with your doctor first before starting a new fitness routine.

Lifestyle Changes to Manage MASH: Change How You Eat
Eat more fruits, vegetables, whole grains, and healthy fats (the unsaturated kind found in olive oil and fish). Avoid drinks and snacks high in sugar and saturated fat. A nutrient-rich diet helps you maintain a healthy weight and lowers your odds of heart disease and other health problems. Not sure what to eat? Use the Mediterranean diet as a guide or ask a dietitian for help.

Lifestyle Changes to Manage MASH: Avoid Alcohol
You don’t get MASH from drinking too much. But chemicals in alcohol can hurt your liver, so it’s safest to stay sober. If you can’t avoid alcohol completely, cut back as much as you can. Some studies show even moderate alcohol use (one drink a day for women, two for men) may boost liver fat and scarring.

Can You Prevent MASH?
There are steps you can take to lower your chances of getting liver disease. Exercise every day. Eat nutrient-rich foods. Control your blood sugar. If you smoke, quit. And check in with your doctor regularly to treat any health conditions that may damage your liver, including diabetes or low thyroid.

Get Vaccinated
Certain viruses raise your odds of liver failure. If you already have MASH, the top two you need to worry about are hepatitis A and hepatitis B. But you may also benefit from vaccines for pneumococcal, COVID-19, flu, Tdap, or others. Ask your doctor which shots are right for you.

What Else Can You Do to Protect Your Liver?
Along with adopting healthy habits, keep your doctor in the loop about all the medication, vitamins, and herbal supplements you take or are curious about. Your liver cleans your blood. And prescription drugs, over-the-counter medicine, or herbal remedies can tax or harm your body’s filter.

Join a Clinical Trial
If you have MASLD or MASH, you may be able to try new treatments before they’re approved for everyone else. Ask your doctor if there’s a clinical trial that would be a good fit for you. You can also find more information about how to participate in research studies through the American Liver Foundation and ClinicalTrials.gov.
Show Sources
IMAGES PROVIDED BY:
1) iStock / Getty Images Plus
2) iStock / Getty Images Plus
3) Westend61 / Getty Images
4) iStock / Getty Images Plus
5) Garry Watson / Science Source
6) Moment / Getty Images
7) Moment / Getty Images
8) iStock / Getty Images Plus
9) iStock / Getty Images Plus
10) svariophoto / Getty Images
11) iStock / Getty Images
12) alejandrophotography / Getty Images
13) SimpleImages / Getty Images
14) The Image Bank / Getty Images
15) Solskin / Getty Images
SOURCES:
National Institute of Diabetes and Digestive and Kidney Diseases: “Definition & Facts of NAFLD & NASH,” “Treatment for NAFLD & NASH,” “Clinical Trials for NAFLD & NASH.”
American Liver Foundation: “NASH Definition & Prevalence,” “Nonalcoholic Steatohepatitis (NASH),” “NASH Treatment.”
UpToDate: “Patient education: Nonalcoholic fatty liver disease (NAFLD), including nonalcoholic steatohepatitis (NASH).”
Endocrinology: “NAFLD and NASH in Postmenopausal Women: Implications for Diagnosis and Treatment.”
American Journal of Gastroenterology: “NASH Leading cause of Liver Transplant in Women: updated analysis of Indications for Liver Transplant and Ethnic and Gender Variances.”
Journal of the Endocrine Society: “PSUN121 Nonalcoholic Steatohepatitis (NASH), Race/Ethnicity, and Gender in Adult US Population of NHANES 17-18.”
Clinical Gastroenterology and Hepatology: “Racial and Ethnic Disparities in Non-alcoholic Fatty Liver Disease Prevalence, Severity, and Outcomes in the United States: A Systematic Review and Meta-analysis.”
JAMA: “Nonalcoholic Steatohepatitis: A Review.”
Cleveland Clinic: “Non-Alcohol Related Steatohepatitis.”
Cedars Sinai: “Non-alcoholic Steatohepatitis (NASH).”
NYU Langone Health: “Five Things You Should Know About Nonalcoholic Fatty Liver Disease.”
UChicago Medicine: “What foods help prevent and reverse fatty liver disease?”
Journal of Clinical and Translational Hepatology: “Drugs for Non-alcoholic Steatohepatitis (NASH): Quest for the Holy Grail.”
Gene Expression: “The Effects of Physical Exercise on Fatty Liver Disease.”
Riley Children’s Health (Indiana University Health): “Nonalcoholic Steatohepatitis (NASH).”
Clinical Liver Disease: “Role of alcohol in nonalcoholic steatohepatitis: Rush university (Con) patients with nonalcoholic steatohepatitis should be abstinent from alcohol use.”
Gastroenterology & Hepatology: “Alcohol Consumption and Nonalcoholic Steatohepatitis/Nonalcoholic Fatty Liver Disease.”
National Cancer Institute Center for Cancer Research: “New insights into why smoking causes fatty liver disease.”
CDC: “Recommended Vaccines for Adults."
FDA: "FDA Approves First Treatment for Patients with Liver Scarring Due to Fatty Liver Disease."