If you have early-stage breast cancer, you may want breast reconstruction after a mastectomy. Some people choose to have their breasts rebuilt with their own tissue instead of with an implant. Your doctor may call this flap surgery.
If you’re considering flap reconstruction versus implants, ask your doctor about the pros and cons of all your choices. They’ll help you pick the right option for your body and lifestyle.
What Is Flap Reconstruction Surgery?
The term “flap” refers to tissue taken from one part of your body that’s used to restore another area. Other terms you may hear are autologous reconstruction or tissue-based reconstruction.
Your doctor can use a tissue flap to rebuild your post-mastectomy breast mound. During flap reconstruction, your surgeon will remove multiple layers of “donor” tissue. This mostly includes skin and fat, but some flap surgeries use muscle. The flap will come from a part of the body that’s similar in makeup to the fibrous and fatty tissue in your breast, which is usually your belly.
There are two different surgical methods used in flap reconstruction, including:
- Free flap. Most often, the surgeon will cut the tissue flap completely out of your body. Once they place it in your chest, they’ll reconnect the original blood vessels to the ones in your breast area. This is where those special skills in microsurgery come in handy.
- Pedicle flap. The surgeon may not cut the original blood vessels in your tissue flap. Instead, they’ll create a tunnel under your skin and move the flap up to your chest that way.
When Do You Get It?
Many people get flap surgery at the same time as their mastectomy (known as immediate reconstruction). But you may need a second surgery later on even if you have reconstruction right away. This is sometimes needed to improve the shape of your reconstructed breast.
In most cases, you can still get flap surgery as a separate procedure from your mastectomy. There are a number of personal and medical reasons for what’s known as delayed reconstruction.
For example, you may not be able to get flap surgery right away if you have inflammatory breast cancer or you need radiation therapy. Or you might want more time to decide if breast reconstruction is right for you. You can ask your doctor what timing is best in your case.
Types of Flap Surgery
There are several different kinds of tissue-based reconstruction. In general, flaps used to rebuild breasts may come from your:
- Belly (most common)
- Inner thighs
- Outer thighs
- Bottom
- Back
- A mix of different places, or the stacked approach
The medical name for each procedure comes from the type of tissue used to rebuild your breast. Some of the more common kinds of flap reconstruction are:
DIEP Flap (belly). This is the type of flap surgery most people get. During this procedure, the surgeon makes a thin cut near your bikini line that goes from hip to hip. They take fat and skin, but no muscle, from your lower belly to rebuild your breast. You can think of this surgery like a tummy tuck.
SIEA Flap (belly). This surgery is a lot like the DIEP flap. The key differences are that your surgeon will take a different section of blood vessels, and they won’t cut the thin layer of tissue (fascia) that covers your belly muscles.
TRAM Flap (belly). Your surgeon may take some of your belly muscle along with fat and skin. You can also get a muscle-sparing TRAM flap, which can help you keep belly strength after surgery.
PAP or TUG. If you don’t have enough tissue in your belly, your doctor may use blood vessels, skin, and fat from your inner thigh. If you get a TUG flap surgery, your doctor will also take some muscle from your upper thigh.
Latissimus dorsi flap. In some cases, your surgeon may need to take tissue from a muscle in your back just below your shoulder. This is something your doctor might suggest if you don’t have enough tissue in your belly or you’ve had flap surgery from another area that’s already failed.
Which Type Should You Get?
The belly is the go-to donor site for flap tissue. But there several things that affect the kind of reconstruction surgery you can get. Some are:
Body type. You’ll need enough tissue in one place that you can spare some for your breast reconstruction. If you’re very thin, your doctor may not be able to take enough from one place like your belly. They may need to build a flap from several spots, including your thigh, butt, or back.
Breast size. You may need to pick a donor site based on how big your breasts are. If you don’t have enough tissue, you can use an implant along with flap reconstruction.
Previous surgeries. Some types of flap reconstruction, like DEIP flap, may not be right for you if you’ve already had surgery on your belly wall. This may include operations like a colostomy or previous tummy tuck.
Desire to get pregnant. Any flap reconstruction that takes muscle from your belly wall, like a TRAM flap, may not be a good choice if you want to have a baby later on. Instead, your doctor may opt to use belly tissue only or to take from donor sites like your thigh or bottom.
Access to specialists. Not all plastic surgeons have the skills needed to do flap surgery well. You may need to travel to another clinic or town to find someone with a lot of experience.
Insurance coverage. Your health insurer must cover breast reconstruction. But they’re not required to pay for the whole thing. Talk to your insurance provider to find out about any copays or out-of-pocket costs that may come with the type of flap surgery you and your doctor think is best.
Pros of Flap Reconstruction
Compared to implants, flap tissue tends to look and feel more like natural breasts. It also moves around with your body and usually lasts a lifetime.
Breasts reconstructed with flap tissue may also:
- Age along with the rest of your body
- Change size and shape when you gain or lose weight
- Stay warm like normal body temperature
- Have white blood cells that can fight infections in your breast
Your immune system also recognizes flap tissue as a part of your own body. This lowers your odds of certain problems that can happen with breast implants. For example, people who get implant-based reconstruction may get hard scar tissue known as a capsular contracture. This can distort how the breast looks and feels.
Cons of Flap Reconstruction
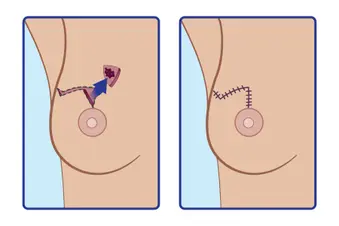
Flap surgery is more complex and requires longer recovery time compared to reconstruction with breast implants. You’ll also have two surgical scars – one at the donor site and one where they rebuild your breast. These scars typically get less noticeable over time but may never disappear.
There’s also a chance you may have problems in the area where your doctor removed healthy tissue, including:
- Belly bulging
- Dimpling or other changes in how your skin looks
- Loss of feeling at the donor site
Some people report weakness, stiffness, or movement problems in the arm that’s on the same side as their mastectomy and reconstruction. Compared to DIEP flap or implant reconstruction, the odds of shoulder problems seem to be higher if you get latissimus dorsi flap surgery.
Are There Risks?
Like all surgeries, flap reconstruction raises your odds of infection and bleeding. You’ll also need to be under anesthesia for a longer period of time compared to implant-based reconstruction.
Rarely, you could have blood flow problems with free flap tissue. For instance, you could get a clot that needs to be repaired with another surgery. If your doctor can’t restore blood flow, the tissue can die. This is known as flap failure, and it’s most likely to happen within the first few days after flap surgery.
Flap surgery may not be right for everyone. Go over all of your health conditions with your doctor. Certain things raise your odds of blood vessel problems or slow wound healing, including older age, diabetes, and obesity. Reconstruction with flap tissue isn’t recommended if you are an active smoker.
What Can You Expect Afterward?
Reconstruction with flap tissue can restore the softness of natural breast tissue. But you’ll likely need a separate surgery if you want to recreate the look and feel of your nipple and areola.
Nerves that were cut during mastectomy may be able to regrow easier through flap tissue compared to around breast implants. But there’s no guarantee that any reconstruction can fully restore the feeling to your chest wall. There’s ongoing research in this area.
Flap reconstruction recovery time is typically longer at first than with breast implants. You’ll need to stay in the hospital for at least 2 to 3 days after surgery so your doctor can make sure there’s good blood flow to your flap tissue.
You may be able to return to work within 2 to 4 weeks. But it may take at least 6 to 8 weeks to get back to your normal activities. That’s because it can take a couple of months for the swelling and bruising to go away.
You’ll have two areas healing at once: your reconstructed breasts and the site of your donor tissue. See your doctor right away if you notice that your breast tissue turns blue or feels cool to the touch. This could be a sign of tissue failure. And let them know if you have any signs of infection, including increased bleeding, worsening pain, or fever.
Show Sources
SOURCES:
Photo Credit: WebMD
Michael Howard, MD, plastic surgeon, Northwestern Medicine Lake Forest Hospital, Lake Forest, IL.
American Cancer Society: “Breast Reconstruction Using Your Own Tissue (Flap Procedures),” “What to Expect After Breast Reconstruction Surgery.”
Yale School of Medicine: “Yale Breast Reconstruction Program.”
National Cancer Institute: “Breast Reconstruction After Mastectomy.”
Memorial Sloan Kettering Cancer Center: “Breast Reconstruction after Mastectomy,” “DIEP Flap Breast Reconstruction Surgery.”
Breastcancer.org: “SIEA Flap,” “Latissimus Dorsi Flap,” “Autologous or “Flap” Reconstruction,” “DIEP Flap,” “TUG Flap,” “PAP Flap,” “Capsular Contracture,” “Latissimus Dorsi Flap Reconstruction Seems to Cause Biggest Loss in Shoulder Stability, Function.”
Epidemiology: “The influence of reconstruction choice and inclusion of radiation therapy on functional shoulder biomechanics in women undergoing mastectomy for breast cancer.”
Mayo Clinic: “Breast reconstruction with flap surgery.”
MD Anderson Cancer Center: “Breast reconstruction options: What to know about DIEP flaps and tissue flaps.”
