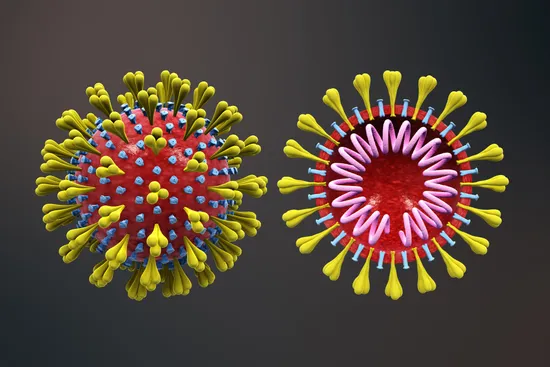
Coronavirus Resource Center
Trusted, comprehensive information and resources for understanding COVID.The Latest in Coronavirus Updates Center
Top Search Terms for Coronavirus
8 million+ Physician Ratings & Reviews
Find Doctors and Dentists Near You
You can also search by physician, practice, or hospital name