Safe Sleep for Baby


Safe Sleep for Your Baby
Your baby needs sleep. And so do you. You’ll both sleep easier if you know what the sleep risks are, and how best to keep your little one safe while they slumber.

Sleeping Risks
All babies under 1 year old are at risk for sudden infant death syndrome (SIDS), especially those younger than 6 months. It has been called crib death because it occurs while baby is sleeping in the crib. It isn’t caused by an infection or a medication, and it can’t be spread. It’s listed as the cause of death if there’s no other explanation. Certain things increase the chances of it. These include:
- Premature birth
- Exposure to alcohol or drugs before birth
- Exposure to smoking before or after birth
- Infection
It’s unclear if having a sibling who died of SIDS increases the risk.
Sometimes a baby’s airway becomes blocked while they sleep. This can lead to sudden unexpected infant death (SUID).

Room Sharing, Not Bed Sharing
The American Academy of Pediatrics now says babies should sleep in their parent’s room for the first 6 months, or better yet, until their first birthday. New statistics say room-sharing can lower the risk of SIDS by as much as 50%. It’s easier to keep an eye on your baby, comfort, and feed them. But they need their own safe space: A bassinet, crib, or co-sleeper (a separate sleeping area that attaches to your bed).Babies should not sleep in the bed with their parents. That increases the risk that the child’s breathing could get cut off, and it’s even more dangerous if you smoke, drink, or take drugs (even some prescription meds.)

Campaign for Safe Sleep
The National Institutes of Health has a public education campaign called Safe to Sleep to reach and inform parents and other caregivers. A lot goes into creating and keeping a secure sleep environment.
Ask your pediatrician about safe sleep at your newborn's first doctor visit.
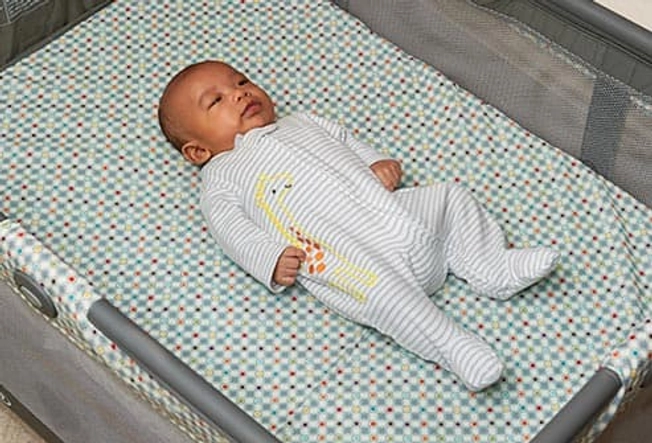
Secure Bedding
Your baby should rest in a crib, co-sleeper, or bassinet that is free of everything except your baby. That means no bumper pads, quilts, blankets, pillows, soft toys, positioning devices, or reachable toys with strings. Make sure the mattress is firm and flat, and always use a tightly fitted sheet. Soft bedding -- above or below your child -- can block their airways.

Less Is More
You may see cribs with stuffed animals, other toys, or pillows in magazines and on TV. They might look cute, but they aren’t safe for your little one.

Safe Sleep Position
Don’t let your baby nap on couches, swings, or any place beside their bed. Every time you put your infant down to get shut-eye, place them in their crib, bassinet, or co-sleeper with their face upward. That’s how your baby should sleep until they can roll from back-to-front and front-to-back. Sleep positioners, like wedges or rolled blankets, may seem like a good idea, but they can move out of place and get in the way of your child’s breathing.
Because of the way babies are built, a healthy infant is less likely to choke when on their back, despite what you may have heard. They are more able to cough out or swallow anything they spit up.

Clothes and Covers
When dressing your baby for bedtime, a one-piece sleeper or sleep sack is the best choice. Depending on the season, it can be lightweight or thick.
It’s best not to use a blanket at all. The wearable blanket should keep them warm. Do not put the baby to sleep in a swaddling blanket.

Breastfeeding and Pacifiers
One of the strongest ways to help prevent SIDS is by breastfeeding your baby. Several studies show that infants who are breastfed, even for a short time, are less likely to get SIDS. Do not breastfeed while sitting in a chair or on a couch if you are tired and in danger of falling asleep yourself.
Pacifiers also lower the risk of SIDS. If you plan to breastfeed, don’t introduce a pacifier until you know your baby is doing well with nursing. Never hang the pacifier around their neck or attach it to their clothes while they sleep. And there’s no need to put it back in their mouth after they have fallen asleep.

Talk to All Caregivers
Don’t assume someone who’s caring for your baby knows how important it is to follow the Safe to Sleep guidelines. Go over those steps with nannies, babysitters, grandparents, and other friends and relatives who care for the infant. Make sure they know they always have to follow the rules. You can even post them in the nursery if you feel better.
