Slideshow: A Visual Guide to Uterine Fibroids

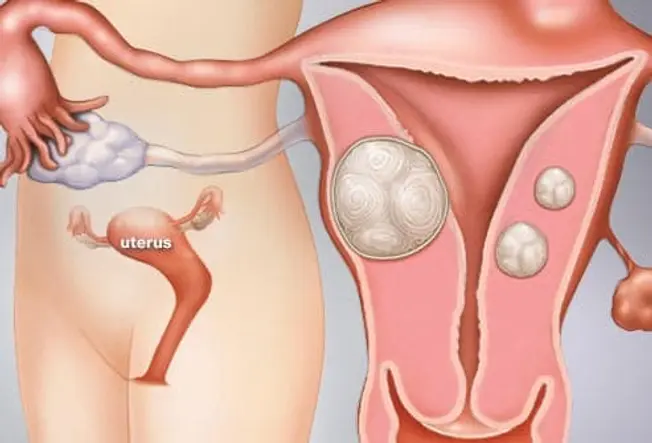
What Are Uterine Fibroids?
Uterine fibroids are noncancerous growths of the muscle tissue of the uterus. Fibroids can range in number and size from a single growth to multiple growths, and from very small to large. As many as 70% to 80% of all women will have fibroids by age 50. The medical term for fibroids is leiomyoma or myoma.
Symptoms of Fibroids: Pressure
Fibroids may cause very mild symptoms, none at all, or symptoms can be severe. In those who do feel symptoms, these uterine growths can cause:
- Pressure on the bladder or rectum
- Frequent urination
- Constipation and/or rectal pain
- Lower back and/or belly pain
If fibroids become very large, they can cause bloating in your belly area, making you look pregnant.

Symptoms of Fibroids: Period Changes
Fibroids may also cause changes to your period, including:
- Mild to severe cramping and pain
- Heavier bleeding, sometimes with blood clots
- Longer or more frequent periods
- Spotting or bleeding between periods
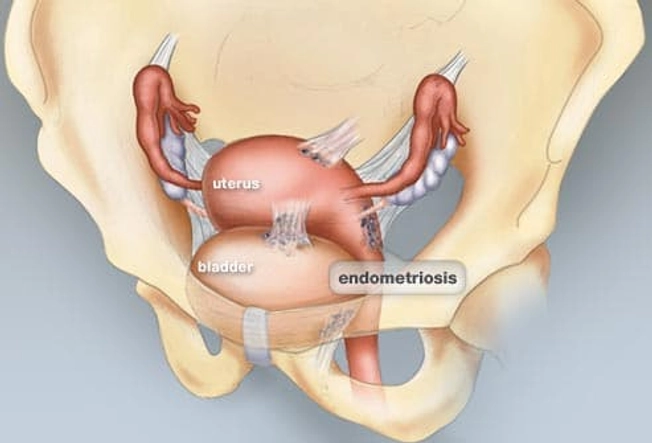
Fibroids or Endometriosis?
Fibroids are one cause of serious menstrual pain, but the pain also can be caused by endometriosis. Endometriosis happens when tissue from the inner lining of your uterus grows in other parts of your body – illustrated here by growths on the outside of the uterus and bladder. This tissue breaks down and bleeds during your period, causing pain during your cycle and painful scar tissue. Fibroids or endometriosis can also cause pain between periods.

What Causes Fibroids?
Doctors don't know exactly what causes fibroids. Their growth has been linked to the female hormones estrogen and progesterone. Studies have found that you're more likely to get fibroids if you started your period at a younger age. Though taking female hormones is linked to fibroids, the use of birth control pills is not.
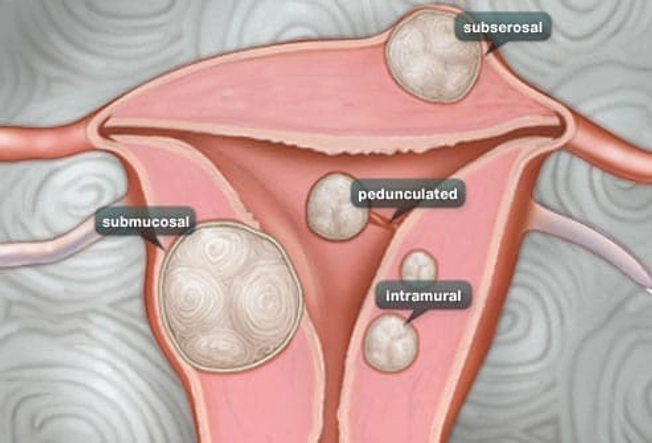
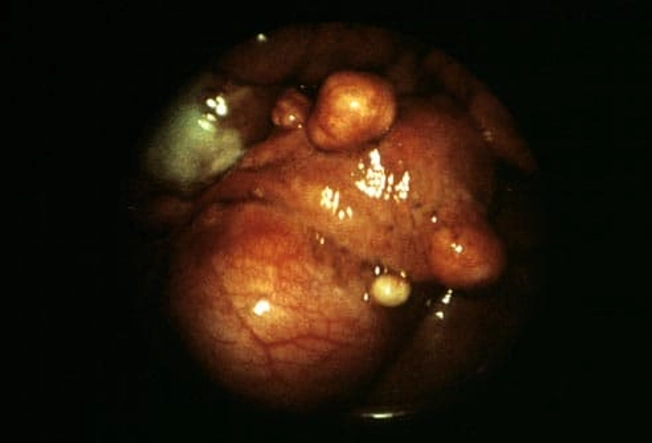
Types of Fibroids
- Intramural fibroids, the most common, grow in the wall of the uterus.
- Subserosal fibroids grow on the outside of the uterus. As they grow larger, they can cause pain due to their size or pressure put on nearby organs.
- Submucosal fibroids grow just underneath the uterine lining. They can crowd into the uterus cavity and lead to heavy bleeding and other more serious complications.
- Pedunculated fibroids grow on small stalks inside or outside the uterus.
You can have more than one type of fibroid.

Who Gets Fibroids?
While it's unclear why fibroids develop, researchers have seen some patterns.
- They usually affect those between the ages of 30 and 40.
- They're more common in Black women.
- They grow more quickly and appear at a younger age in Black people than in White people.
- Having a family member with fibroids increases your risk.
- Being overweight or obese and having high blood pressure also may increase your risk.

Complications: Fibroids and Anemia
Some women with fibroids who have unusually heavy bleeding during their periods may become anemic. Many cases of anemia due to iron deficiency from periods are mild and can be treated with a change in diet and iron supplement pills. Untreated anemia can lead to extreme tiredness and lack of energy – and, in serious cases, heart problems.

Complications: Getting Pregnant
Fibroids don't usually interfere with fertility and pregnancy. But some people with fibroids have more pregnancy complications and delivery risks. Fibroids may cause the baby to be in an abnormal position and can cause early labor. They may also cause pelvic pain and heavy bleeding after delivery, which may require surgery. In some cases, fibroids could block your fallopian tubes. Fibroids growing along the inner uterine wall may make it harder for a fertilized egg to attach.

When to See a Doctor
See your health care provider if you have any of the following fibroid symptoms:
- Heavy bleeding during your period
- Periods that have become more painful
- Frequent peeing, or if you can't control the flow of urine
- A change in the length of your period over three to six cycles
- New, long-lasting pain or heaviness in your lower belly or pelvis
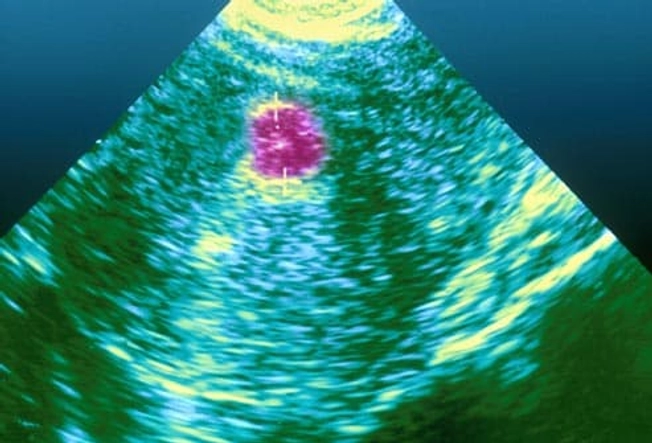
Diagnosis: Exam and Imaging
Your doctor may feel moderate and large uterine fibroids during a routine pelvic exam. Tests, such as an ultrasound, can give them information about the size and location of other fibroids. If you have fibroids and are trying to get pregnant, a test called a hysterosalpingogram will show an outline of your uterus and fallopian tubes and may detect abnormalities. You may also need other imaging procedures to show your doctor the inside of your uterus or belly.

Treatment: Pain Medication
Pain medications, such as acetaminophen, and nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, can help relieve menstrual cramping.

Treatment: Birth Control
Oral contraceptives manage levels of estrogen and progestin. This usually leads to lighter periods and can ease some symptoms of fibroids, such as heavy bleeding and cramping. Other hormonal birth control methods that may lessen fibroid symptoms include progestin shots or progestin-releasing IUDs.

Other Hormone Therapies
Drugs called gonadotropin-releasing hormone (GnRH) agonists or GnRH antagonists offer temporary symptom relief by stopping or reducing your periods and shrinking fibroids. These drugs block your body's production of estrogen, so they could also cause bone loss, hot flashes, and vaginal dryness. They're not meant to be taken long-term. Fibroids will return to their previous size once you stop taking them. These may be used to shrink fibroids before fibroid removal surgery.
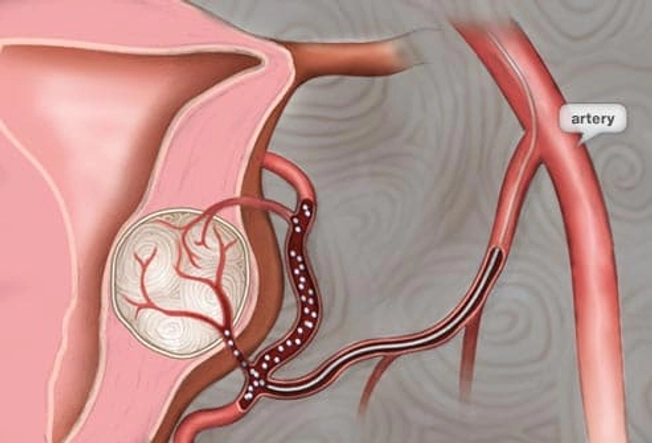
Treatment: Embolization
For mild to moderate symptoms, uterine fibroid embolization may be a good option. In this procedure, your doctor guides a catheter to the uterine artery. Tiny particles of plastic or gelatin are then released into the blood vessels that feed the fibroid, causing it to shrink over time. If you plan to get pregnant later on, embolization is not for you.

Treatment: Surgery
A myomectomy generally removes the largest fibroids. It’s an option if you still want to have children. In a hysterectomy, your uterus is removed, meaning you can no longer get pregnant. Endometrial ablation, which is good for treating smaller fibroids, destroys the lining of your uterus, so pregnancy isn't possible afterward.
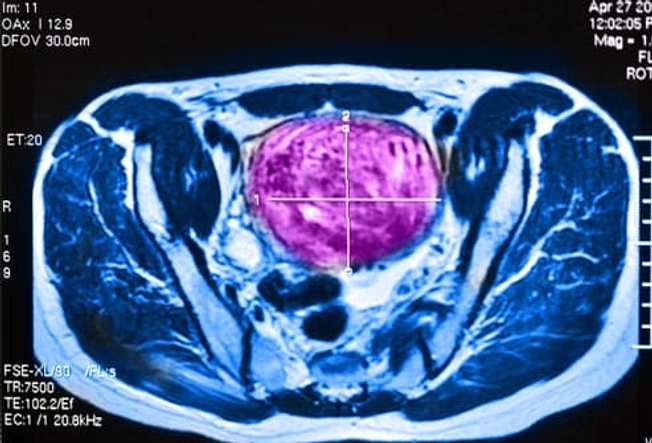
Treatment: Ultrasound
Ultrasound is one way to destroy fibroids without the risk of damaging your uterus. The treatment uses high-intensity ultrasound waves to kill the fibroid tissue. This procedure has a quick recovery time. You may be able to return to your regular activities within 24 hours. The long-term effects are still being studied. It's not recommended if you want to become pregnant.

Fibroid Remedy: Exercise
Regular exercise may prevent fibroids. In one study, women who exercised 7 or more hours a week had fewer fibroids than those who exercised less than 2 hours a week. Obesity also increases your risk for fibroids. Exercising regularly can help you maintain a healthy weight and reduce the chances that you'll get fibroids.

Care for Anemia
If you have fibroids and don't get enough iron in your diet, you could get anemia, a condition in which your body has fewer red blood cells than normal. Symptoms include tiredness, chest pain, and shortness of breath. Treatment may include eating more iron-rich foods, such as meats, poultry, fish, leafy greens, legumes, and iron-fortified breads and cereals. Your doctor also may suggest iron supplements.