Raynaud’s Phenomenon and Raynaud’s Disease

Raynaud’s Phenomenon
This condition causes “attacks” that limit blood supply to fingers and toes, which may get pale, cold and numb. As blood returns, they may start to tingle and hurt. Except in rare cases, it’s typically not serious. There’s no cure, but there are changes you can make to your routine, dress, and diet that can help you manage symptoms.

Primary vs. Secondary Raynaud’s
Primary Raynaud’s happens by itself without any obvious cause. Secondary Raynaud’s happens as a symptom of an underlying illness or injury. Only your doctor can determine which one you have. In either case, you may see it called Raynaud’s “disease,” or “syndrome,” or “phenomenon.” These terms are often used interchangeably, but technically, Raynaud’s disease refers only to the primary form.

Cause
The cause is unclear. Even though another illness can bring on secondary Raynaud’s, doctors don’t know exactly what leads to the symptoms of the condition. They do know that they typically happen when blood vessels overreact and spasm in response to low temperatures, stress, or high emotions.

Primary Raynaud’s
This is the most common form of the condition. It typically shows up between the ages of 15 and 30. Primary Raynaud’s tends to be less serious than the secondary type. It doesn’t have a link to another medical condition, and if you have it, you’re not likely to develop one later. Symptoms may be so mild that you don’t feel the need to seek treatment. Sometimes, they get better on their own.

Secondary Raynaud’s
This form of Raynaud’s tends to show up later, around age 40. It can cause more serious symptoms than the primary kind. The root cause could be:
- Diseases that damage arteries, nearby nerves, and connective tissue, especially in your hands and feet
- Repeated movements or injury that damages nerves around blood vessels near your feet or hands
- Medicines that change your blood pressure or narrow your blood vessels

Common Underlying Conditions
Scleroderma, an inflammatory autoimmune disease that hardens connective tissue, is the most common cause of secondary Raynaud’s. Other autoimmune disorders, like lupus, rheumatoid arthritis, and Sjögren's syndrome, may also do it. A few other conditions that can play a role include:
- Hardening of the arteries (atherosclerosis)
- Pulmonary hypertension
- Blood disorders (cryoglobulinemia, polycythemia)
- Thyroid problems

Symptoms
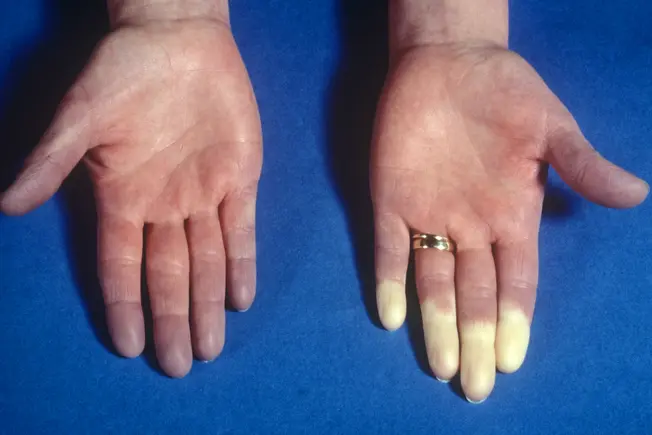
An “attack” usually hits the fingers and toes, but can also strike your nose, ears, nipples, or lips. It might start in one finger or toe and move on to others. It may last less than a minute, or go on for hours. Affected areas might:
- Turn pale, white or even blue in color
- Feel numb, cold, or painful
- Throb, burn, tingle, and swell when blood returns
Serious cases of secondary Raynaud’s can cause sores. Rarely, they can even kill living tissue (gangrene).

Who Gets Primary Raynaud’s?
- Female sex: Women get it more than men.
- Climate: It’s more common in people who live in colder climates.
- Age: Anyone can get it, but it’s more common between 15 and 30.
- Genetics: You’re more likely to have it if a brother, sister, or parent has it.

Who Gets Secondary Raynaud's?
Having an autoimmune disease like scleroderma and lupus makes it more likely that you’ll have Raynaud’s. Other things that can raise your chances include:
- Being older than 30
- Jobs that use repeated motions, like typing or hammering, or vibrating tools, like buffers and jackhammers
- Exposure to certain chemicals like vinyl chloride, found in PVC plastics
- Living in a cold climate
- Smoking

Diagnosis
When you see your doctor, they’ll examine you and take your medical history. They may put your hands in ice water briefly to see how long it takes for them to warm up to a normal temperature. They could also look at your fingers under a microscope to see the tiny blood vessels in your fingernails. Other tests, including blood tests, can help show whether your Raynaud’s is primary or secondary.

Treatment: Protection From the Cold
You may be able to manage your Raynaud’s symptoms on your own. Start by protecting yourself from the cold:
- Wear multiple layers of clothing so you can adjust when necessary.
- Wear a hat, scarf, mittens, and warm socks in cold weather.
- Keep hand and foot warming packs on you to be prepared for extra cold weather.
- Start the car to warm it up before you drive in cold weather.
- Wear gloves to take food out of the fridge and freezer.

What to Do During an Attack
If you have a Raynaud’s attack, you can make it less severe and lessen its length by warming the affected areas. To quickly warm your fingers and toes:
- Rub your hands and feet.
- Tuck your hands in your underarms.
- Run warm -- not hot -- water over your hands and feet.
- Wiggle your fingers and toes.
- If you’re stressed, step back and relax.

Treatment: Avoid Other Triggers
There are other triggers besides cold temperatures that you can try to avoid:
- Vibrating tools like drills and sanders
- Repeated motions like typing or hammering
- Industrial chemicals
- Caffeine, alcohol, and smoking
- Stress

Treatment: Adjust Medication
Certain medications can trigger or worsen symptoms of Raynaud’s, especially ones that narrow your arteries or affect blood flow. These may include:
- Over-the-counter allergy and cold pills
- Blood pressure meds called beta-blockers
- Migraine meds
- Some diet aids
- Birth control pills
- Some cancer drugs
Talk to your doctor about your meds, especially before you make any changes.

Treatment: Medicine and Surgery
If your symptoms interfere with daily life even after you make changes to your routine, clothing, and other habits, your doctor may be able to help with medication such as:
- Calcium channel blockers
- Alpha blockers
- Prescription skin creams
- ACE inhibitors
In rare cases, you may need shots or surgery to help improve blood flow and prevent tissue damage.