When Back Pain Is More Than General Arthritis
Hide Video Transcript
Video Transcript
JOHN WHYTE
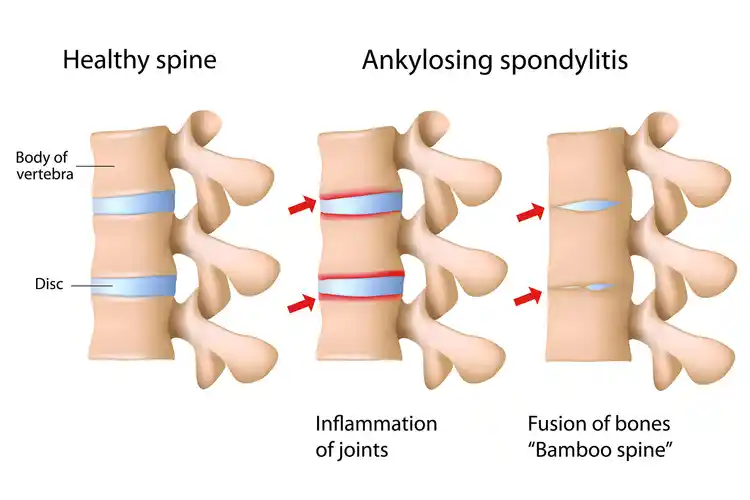
Welcome, everyone. I'm Dr. John Whyte, the chief medical officer at WebMD. Ankylosing spondylitis is a type of arthritis that causes pain and stiffness in your spine. It usually starts in your lower back but can also progress to your neck and destroy other joints in other parts of your body. Now, in medicine we often make words so complicated. So to break it down for you, "ankylosing" means fused bones. "Spondylitis" means inflammation of the vertebra. There is no cure for AS. But we do know that there are effective treatments and exercise can help as well. But you first need to recognize if you have ankylosing spondylitis and get the right diagnosis.
So helping me to unpack it all are two experts. Joining me is Dr. Marina Magrey. She's Division Chief of Rheumatology at University Hospitals Cleveland Medical Center, and Dr. Maureen Dubreuil. She's Assistant Professor of Medicine at Boston University. Doctors, thanks for joining me.
MARINA MAGREY
Thank you for having us. MAUREEN DUBREUIL
Thanks for having us JOHN WHYTE
Dr. Magrey, I want to start with you. I mentioned what the words mean. But help viewers understand. What typically are the symptoms that someone has with ankylosing spondylitis? MARINA MAGREY
So the most common symptom the patient has is low back pain which usually starts before the age of 45 years. The back pain is usually insidious or slow in onset. And it's chronic-- lasting for three or more months. And in addition to that, these patients can also have neck pain, chest wall pain. About 30% to 40% of these patients can have peripheral joint involvement-- predominantly, the joints of the lower extremities. They may have a swollen knee or a swollen ankle and hip pain.
These patients also tend to have something what we call enthesitis, which is where the tendons and ligaments attach to the bones. They have inflammation at those sites and will have pain in these sites. Particularly, they may have pain on the sides of their hips, elbows, shoulders, chest wall. And very rarely in patients with ankylosing spondylitis, they may develop swollen digits and toes which look like sausages.
JOHN WHYTE
So I'm an internist. I see back pain all the time with patients. So I want to delve in a little deeper because that classically, as you point out, is one of the first symptoms. So Dr. Magrey, what's different about the back pain and ankylosing spondylitis, versus general arthritis or lumbar sprain or sciatica? MARINA MAGREY: The characteristic features of back pain in ankylosing spondylitis is they have inflammatory back pain, which means that this back pain is associated with morning stiffness that usually lasts more than 30 minutes. The back pain gets better with activity. If you ask them as the day goes by if they're up and about, they often mention that the back pain is better. And it gets usually worse or does not improve by sitting.
JOHN WHYTE
So Dr. Dubreuil, it's much more than just back pain. So we don't want people to think, hey, if they have back pain, they might have ankylosing spondylitis. It occurs earlier in life than some other type of arthritis. Do we know what causes it or who might be at more risk? MAUREEN DUBREUIL
Sure. Well we do have some information about what causes ankylosing spondylitis and other forms of axial spondyloarthritis. We think this is a highly genetic-driven disease, with the primary gene involved at this time, we know is HLA-B27. HLA-B27 codes for a protein that is on the surface of inflammation, blood cells. And in the presence of this gene, we know that it promotes inflammation through interaction of different inflammatory cells. We believe that women and men are equally affected and there's no specific group of people more likely to get the disease.
JOHN WHYTE
And Dr. Magrey, a patient comes to you. You're starting to think, hey, this might be ankylosing spondylitis. What lab tests or imaging studies are you going to order? MARINA MAGREY
It's a clinical diagnosis. So we rely on a comprehensive history of this patient. So based on our clinical suspicion is high, there is no any specific blood test which helps us to make this diagnosis. But there are certain tests we order that may aid us. Like we will order some markers of inflammation-- c-reactive protein, ESR. And if they are elevated, they may increase our diagnostic probability that this patient may have ankylosing spondylitis. But they're only elevated in about, I would say 50% to 60% of these patients.
We do order this genetic test, blood test, HLA-B27, looking if the gene is positive. But all patients may not have the gene. Particularly, African-Americans and minorities. The prevalence of HLA-B27 is much lower in them. And then we usually start with an X-ray of the pelvis because it's believed that the disease starts probably in SI joints, the sacroiliac joints. And that's the first test which we order.
JOHN WHYTE
Didn't they used to say, historically, bamboo spine? Tell us about that. MARINA MAGREY
So that's the end stage of the disease, when the spine is completely fused. The good news is that in these days, we are not seeing many patients with bamboo spines because there has been a significant advancement in the treatment of this disease. We have multiple medications now available which are capable of preventing that bamboo spine. JOHN WHYTE
So you order the X-ray, the plain film, the sacroiliac joint. Anything else? MARINA MAGREY
So that's the first test. Now, that's the gold standard for making this diagnosis. If the X-ray shows us damage in the SI joint, then we call it ankylosing spondylitis or radiographic axial spondyloarthritis. There are patients in which their X-ray may be normal. Because it takes about 7 to 10 years for these changes to show on an X-ray. So in those patients, we order an MRI of the SI joints. And usually, what we request is MRI of the SI joints with two particular sequences-- T1 and a STIR sequence, looking for bone marrow edema in these SI joints.
JOHN WHYTE
And Dr. Dubreuil, what are the complications of this condition? How does it impact the quality of life for patients? MAUREEN DUBREUIL
Well, as you can imagine, having inflammation and chronic back pain does impact people's quality of life quite dramatically. So people have limitations and their ability to function in activities of-- sometimes activities of daily living. Sometimes limitations in their jobs or their social roles. One of the more common impacts is related to sleep in that people have disrupted sleep, and therefore have fatigue. So it is very important in terms of its impact on quality of life, regardless of whether a person has ankylosing spondylitis or another form of axial spondyloarthritis arthritis.
JOHN WHYTE
So a patient has back pain, Dr. Dubreuil. Should they be concerned at all about ankylosing spondylitis if they're young? If other family members had back pain early on? Or do they need to be waiting until they develop some of these other conditions that might give them a greater hint that, yes, this is the reason why. What's your message to viewers? MAUREEN DUBREUIL: For young people who have chronic back pain, especially if it has some of the inflammatory features that Dr. Magrey mentioned, they should address it with their primary care physician first. One of the more common treatments to begin with is physical therapy. And other common treatments can be tried. But if that pain persists, despite those common treatments, then yes, it may be time to have a workup with a rheumatologist.
JOHN WHYTE
You have to see your rheumatologist for this diagnosis? MAUREEN DUBREUIL: So rheumatologists are the best people to make the diagnosis because we're the experts in inflammation type of arthritis.
JOHN WHYTE
Well, doctors I want to thank you both for helping us to understand what are the signs and symptoms of ankylosing spondylitis and what tests you might need to make sure you're going to get the best care. Thanks for joining me. MAUREEN DUBREUIL
Thank you. [MUSIC PLAYING] 