Mantle Cell Lymphoma Stages and Treatments

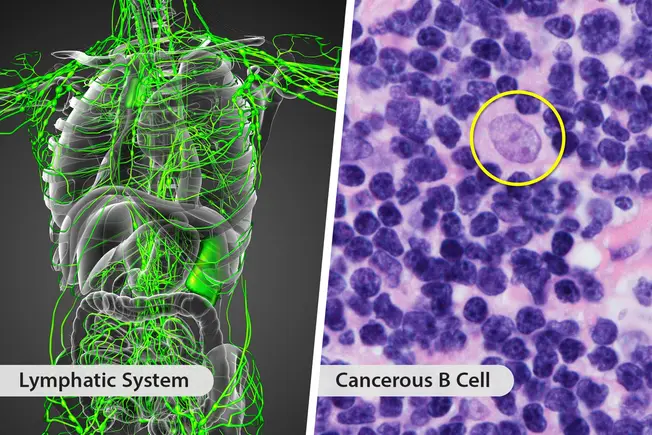
What Is Mantle Cell Lymphoma?
It’s a type of non-Hodgkin’s lymphoma. This means it affects your lymphatic system, which is part of your immune system. It forms in an area of your lymph nodes called the mantle zone. It takes over your B Cells, which normally make antibodies to fight infections. The cancerous B cells grow out of control and make your lymph nodes larger. The cancer can spread to your bone marrow, liver, and gastrointestinal tract.

Symptoms
Some people with mantle cell lymphoma have no obvious symptoms. This can delay a diagnosis. Others notice signs like weight loss, night sweats, fever, fatigue, nausea, and belly pain or bloating.

Who’s at Risk?
Mantle cell lymphoma is a rare cancer. It makes up only 6% of all non-Hodgkin’s lymphomas. It mostly affects men over 60. White men are at a higher risk than black men. The cause is usually damage to your DNA instead of something you’ve inherited in your genes.

How It Progresses
Once you have a diagnosis, your doctor will check your cancer stage. This tells how much the cancer has spread. If you’re at:
- Stage I: The cancer is in one lymph node or group of lymph nodes next to each other.
- Stage II: It’s in two or more lymph nodes or groups of lymph nodes next to each other on the same side of the diaphragm.
- Stage III: It’s in lymph nodes on both sides of your diaphragm or nodes above your diaphragm and in your spleen.
- Stage IV: It’s widespread.

Treatment
Most often, you’ll get chemotherapy and immunotherapy. Your doctor may also use radiation therapy, targeted therapy, and stem cell transplants. Surgery usually isn’t helpful. Your exact treatment plan will depend on many things. These include what stage your cancer is in, your overall health, and your age.

Chemotherapy
Cancerous B cells can travel through your bloodstream and spread. But chemotherapy drugs also travel through your bloodstream to kill cancer cells wherever they’re found. You’ll usually get a combination of drugs that includes rituximab (Rituxan). You’ll get the drugs through an IV.

Immunotherapy
Immunotherapy drugs use the natural disease-fighting power of your immune system. Some drugs attach to the surface of cancer cells so it’s easier for your immune system to find and kill them. Others boost the natural ability of your immune system cells (T cells) to fight cancer. Immunotherapy is often used with chemotherapy.

Radiation
This treatment uses X-rays to kill cancer cells and shrink tumors. It will target a very specific area of your body, usually your lymph nodes. The treatment is quick and painless, but side effects like skin reactions and tiredness are common. You’ll usually get several small doses over the course of a few weeks. Doctors often use radiation when your cancer doesn’t respond to chemotherapy.

CAR T-Cell Therapy
This type of immunotherapy uses your body’s cells. Your doctor will draw blood to collect T Cells, immune cells that fight infections. In a lab, they’ll change the cells so they make “chimeric antigen receptors” (CAR) on their surface. Then your doctor will put them back into your body, where they fight your lymphoma. Doctors often use this therapy if your cancer comes back after treatment or doesn’t respond to chemo or immunotherapy.

Targeted Therapy
If your cancer comes back or doesn’t respond to chemo or immunotherapy, you may get targeted therapy. It uses drugs that stop or slow tumor growth by acting on specific molecules in cancer cells. This is different from chemotherapy, which kills any quickly dividing cell, whether it’s normal or cancerous. Targeted therapy drugs often come in pills.

Stem Cell Transplant
Your bone marrow, the spongy material inside your bones, contains immature cells called stem cells that grow into blood cells. They can replace cells that chemotherapy kills. This lets your doctor use stronger chemotherapy than they would if stem cells weren’t available. Stem cell transplants and high-dose chemotherapy can tax your body. Your doctor will usually only suggest them if your lymphoma is aggressive or returns after treatment.

Watch and Wait
A small number of people with mantle cell lymphoma have what’s called slow-growing (indolent) MCL. If this is the type that you have, your doctor may suggest that you don’t jump into treatment. This lets you avoid the side effects. Instead, they’ll have you visit every 2-3 months and have an imaging test every 3-6 months. You’ll only need treatment if your cancer spreads or your symptoms get worse.

Outlook
Most people respond well to their first round of chemotherapy. Often, they go an average of 20 months without their cancer getting worse. If you have mantle cell lymphoma, you can expect to live about 8 to 10 years, but you can live for 20 or more.