Visual Guide to Pancreatic Cancer

What It Is
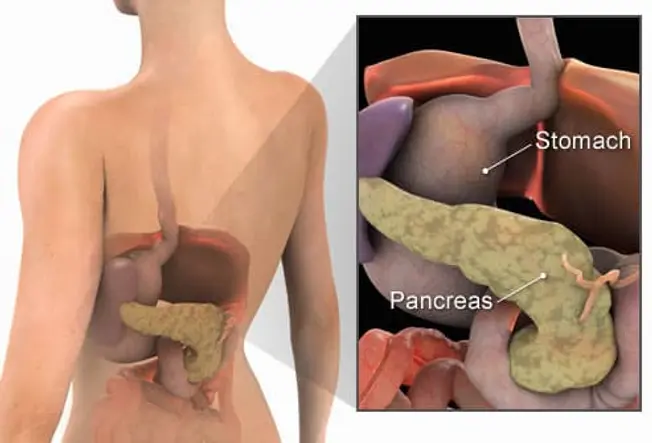
Pancreatic cancer happens when malignant (cancerous) cells grow, divide, and spread in the pancreas. The pancreas is a 6-inch-long, spongy, tube-shaped organ located in the back of the abdomen, behind the stomach. It has two major jobs in the body: to make digestive juices (called enzymes) that help break down food, and to make hormones -- including insulin -- that control the body's use of sugars and starches.

In the Headlines
Jeopardy host Alex Trebek, Supreme Court Justice Ruth Bader Ginsburg, Apple co-founder Steve Jobs, and actor Patrick Swayze are among those who have died of pancreatic cancer.
Symptoms
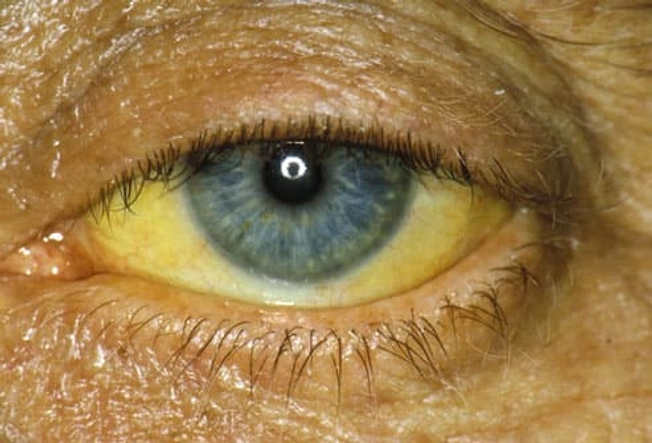
People often don’t have symptoms in the early stages of this disease. But as the cancer grows and spreads, pain often develops in the upper abdomen and sometimes spreads to the back. The pain may worsen after you eat or lie down. Other symptoms may include jaundice, nausea, loss of appetite, weight loss, fatigue, weakness, and depression.

Survival Rates: What to Know
Because doctors rarely find pancreatic cancer in its early stages when it’s easiest to treat, it’s one of the most deadly cancers. About 9% of people with pancreatic cancer live at least 5 years after diagnosis. But the 5-year survival rate is much better -- 44% -- if it hasn’t spread past the pancreas. Know that survival rates can’t predict what will happen to any single person and may not reflect newer types of treatment.

Causes
Experts don’t know the exact cause of pancreatic cancer. Certain gene mutations can cause it. Other risk factors include smoking, age (it’s usually diagnosed in people older than 45), diabetes, chronic pancreatitis due to a genetic mutation, liver cirrhosis, family history of the condition, gender (it’s more common in men than women), obesity, certain chemicals, and race. (African Americans have a slightly higher risk than whites; experts don’t know why.)
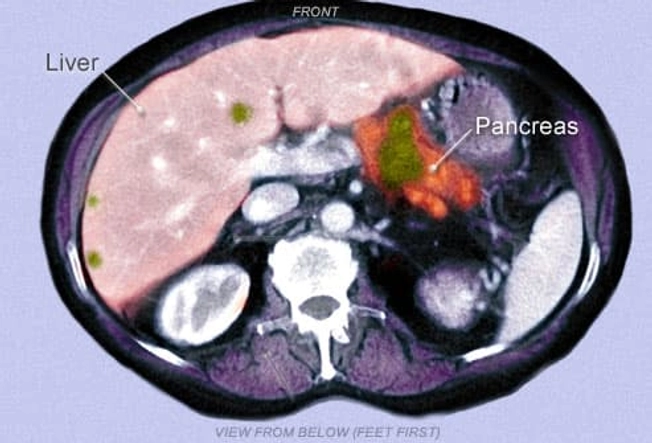
Diagnosis
It can be hard to find this disease early on. A doctor may not see or feel a small tumor during a routine exam. To help make the diagnosis, you may get imaging tests such as an ultrasound or CT scan. The green area shown in this CT scan appears to be cancer in the pancreas and liver. These studies also help your doctor choose the most appropriate treatment. For a diagnosis, you’ll get a biopsy, in which your doctor uses a needle or does an operation to take a bit of tissue from the tumor for testing.

Surgery
Surgery to remove the tumor can cure the cancer if it hasn’t spread past the pancreas. Your surgeon will keep as much of the normal pancreas intact as possible. Unfortunately, with pancreatic cancer, the cancerous cells usually have spread past the pancreas by the time of diagnosis. If the tumor is too large to remove, a different type of surgery might be an option. The goal would be to help ease some of the symptoms and prevent certain problems related to the size of the cancerous mass.

Radiation Therapy
Radiation therapy uses high-powered radiation to kill cancer cells. For pancreatic cancer, you’d likely get it 5 days a week for several weeks. This schedule helps to protect normal tissue by spreading out the total dose of radiation. Radiation is also being studied as a way to kill cancer cells that stay in the area after surgery. Radiation therapy can help relieve pain or digestive problems caused by large tumors.

Chemotherapy
Chemotherapy uses drugs to destroy cancer cells and stop them from growing or multiplying. It may involve one drug or a combination of drugs. You may get it by mouth or by injection. The drugs enter the bloodstream and travel through the body, making chemotherapy a good choice for cancer that has spread. You may also get it after surgery to kill any cancer cells left behind.
Targeted Therapy
These medications attack specific parts of the cancer cells. Targeted therapies seem to have fewer side effects than chemotherapy and are less harmful to normal cells. Doctors can use a targeted therapy called erlotinib (Tarceva) along with chemo to treat advanced pancreatic cancer. Side effects can include a rash, diarrhea, appetite loss, and fatigue.
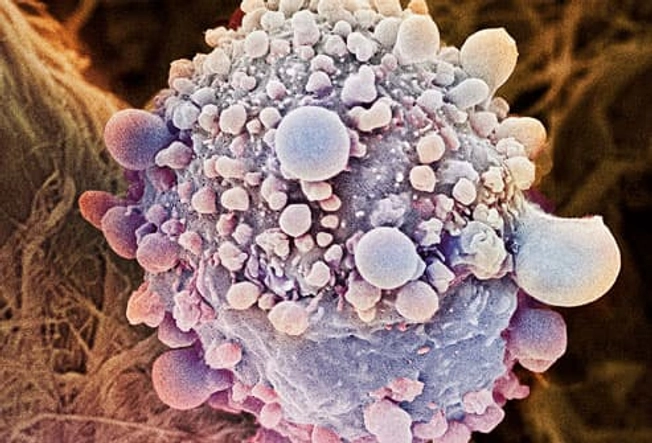
Shown here is a color enhanced, magnified view of a pancreatic cancer cell.
Immunotherapy
This type of treatment uses your immune system to fight disease. For pancreatic cancer, doctors can use pembrolizumab (Keytruda) to block a protein called PD-1 so that the immune system can attack the cancer. Side effects can include fatigue, skin problems, joint pain, and gut problems (constipation, diarrhea, and nausea). More serious side effects can happen if the immune system starts to attack the body itself.

Palliative Care
Palliative therapy is used to ease symptoms and manage pain in any stage of the disease. You can get it along with other medical treatments. The goal is to improve quality of life not just in the body, but in the mind and spirit. While palliative therapies are clearly appropriate at the very advanced stages of the disease, they also help when given along with other treatments that target the cancer.

Get Support
There are many resources to help you and your loved ones as you manage your pancreatic cancer, including these organizations:
- Pancreatic Cancer Action Network helpline: 877-272-6226
- American Cancer Society: 800-227-2345
- Cancer Care: 800-813-HOPE (4673)

Can You Prevent Pancreatic Cancer?
While there’s no way to prevent all cases, you can take action against the risk factors you can control. The American Cancer Society’s tips:
- If you smoke, quit now.
- Get to a healthy weight and be physically active.
- Eat a healthy diet, focusing especially on plant foods.
- If you drink alcohol, keep it moderate. Heavy drinking may be a risk factor.