The Right Treatment for Your Goal
Hide Video Transcript
Video Transcript
[MUSIC PLAYING]
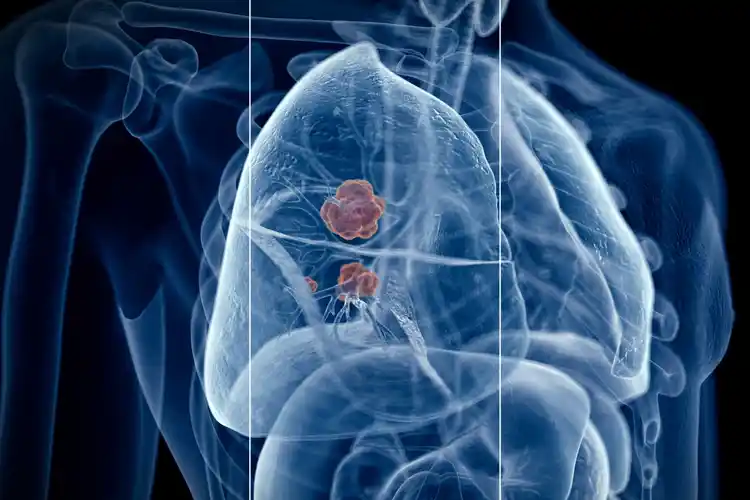
We know that lung cancer is still the most common cause of cancer in the United States. And although a diagnosis of inoperable lung cancer is serious, there are various options for treatment. Some of these treatments may slow or reverse disease progression. They may ease symptoms or even lengthen a patient's life. These treatments can include chemotherapy, radiation therapy, immunotherapy, photodynamic therapy. In addition, there's a host of research going on to find the best therapies.
Joining me to discuss all of this is Dr. Joseph Murray, he's the co-director of the Lung Cancer Precision Medicine Center of Excellence at Johns Hopkins Medicine, And Dr. Melinda Hsu, she's a thoracic medical oncologist and assistant professor of hematology oncology at Case Comprehensive Cancer Center, University Hospitals in Seidman Cancer Center. Doctors, thanks for joining me.
However, for the vast majority of inoperable lung cancers, these patients present with very advanced and metastatic disease. And for those patients, the upfront considerations, including the appropriate testing of their tumor type as well as the features of their tumor that would indicate what type of systemic therapy or therapy that treats their whole body, is truly indicated.
And for the patients who have metastatic or stage IV disease, I also focus on the fact that we can still treat their cancer. And that it's not that we are just trying to treat them for no reason, but the reason to treat their cancer is to help them live for longer and to help improve whatever symptoms they have from their cancer and also maintain or improve their quality of life.
Systemic therapy means we're using a therapy that treats the cancer throughout their body. And patients may be most familiar and viewers may have heard most commonly about chemotherapy, an infusion therapy that's given through a vein and a catheter that's placed in a vein. There are other types of treatment we use through the vein as well, including immunotherapy.
But there's also a category of therapies that we give as oral medications, just like pills and vitamins you might take for other conditions. And this expanse and options for treatment are critical to identify to match a patient with their appropriate therapy and, as Dr. Hsu mentioned, to tailor that in the setting of their other medical conditions.
And the way I describe this to patients is I don't want to just give them the first therapy I have available, I want to give them the best therapy that provides them ultimately the best outcomes over their life. And so my focus is on getting this testing done as efficiently as possible. And I use a combination of tissue and liquid biopsy testing to complete this comprehensive molecular profiling. I think that this can afford us avenues to increase the breadth and speed with which we can complete this testing for patients.
[MUSIC PLAYING]
JOHN WHYTE
Welcome, everyone. I'm Dr. John Whyte and the Chief Medical Officer at WebMD. And today, we're going to talk about inoperable lung cancer, specifically what treatments might be available if you or a loved one get that diagnosis. We know that lung cancer is still the most common cause of cancer in the United States. And although a diagnosis of inoperable lung cancer is serious, there are various options for treatment. Some of these treatments may slow or reverse disease progression. They may ease symptoms or even lengthen a patient's life. These treatments can include chemotherapy, radiation therapy, immunotherapy, photodynamic therapy. In addition, there's a host of research going on to find the best therapies.
Joining me to discuss all of this is Dr. Joseph Murray, he's the co-director of the Lung Cancer Precision Medicine Center of Excellence at Johns Hopkins Medicine, And Dr. Melinda Hsu, she's a thoracic medical oncologist and assistant professor of hematology oncology at Case Comprehensive Cancer Center, University Hospitals in Seidman Cancer Center. Doctors, thanks for joining me.
MELINDA HSU
Thanks for having us. JOSEPH MURRAY
Thank you. JOHN WHYTE
Well, let's start off with, what are some of the treatments when a patient is told that their lung cancer is inoperable? Dr. Murray, what's the thought process that you go through? JOSEPH MURRAY
So the first step is assessing what is the next best option for the patient. And this involves, as you noted, a combination of specialists, who can provide different sorts of therapy to a patient to treat their lung cancer. One thing to consider upfront is whether we can use a definitive treatment paradigm, combining chemotherapy with radiation therapy, in hopes of affording even the potential for a cure for locally advanced lung cancers. However, for the vast majority of inoperable lung cancers, these patients present with very advanced and metastatic disease. And for those patients, the upfront considerations, including the appropriate testing of their tumor type as well as the features of their tumor that would indicate what type of systemic therapy or therapy that treats their whole body, is truly indicated.
JOHN WHYTE
Dr. Hsu, what do you find is the patient's mindset when they're told that it's inoperable, yet here, we still have these treatments? In some ways, it almost seems to be overly confusing to patients, or are we using the right language, right? Because inoperable doesn't mean that there aren't treatments, it just means that there's not a surgical therapy. But there still can be many options to address their disease. Is that right? MELINDA HSU
Absolutely. And I agree that it can be confusing. And a lot of patients have in their mind that they just want the cancer out, and the only way to achieve that is through surgery. And so for the patients with locally advanced cancer, where we can still offer a definitive treatment to try to cure their cancer, I make sure to explain that we are still trying to cure their cancer with a combination of radiation and systemic treatment, like Dr. Murray mentioned. And for the patients who have metastatic or stage IV disease, I also focus on the fact that we can still treat their cancer. And that it's not that we are just trying to treat them for no reason, but the reason to treat their cancer is to help them live for longer and to help improve whatever symptoms they have from their cancer and also maintain or improve their quality of life.
JOHN WHYTE
Dr. Murray, what does treatment provide for patients? We've had amazing advances in terms of the options that we have available. How do we help patients think about treatment for inoperable lung cancer? JOSEPH MURRAY
This is a challenge, especially early in a patient's diagnosis, where they just want to know that there is some hope. And so the way I try to frame that is based on what I know about the details of their cancer. And I'm going to focus on those patients for which we first start with systemic therapy, the category of patients that have metastatic disease at time of diagnosis. Systemic therapy means we're using a therapy that treats the cancer throughout their body. And patients may be most familiar and viewers may have heard most commonly about chemotherapy, an infusion therapy that's given through a vein and a catheter that's placed in a vein. There are other types of treatment we use through the vein as well, including immunotherapy.
But there's also a category of therapies that we give as oral medications, just like pills and vitamins you might take for other conditions. And this expanse and options for treatment are critical to identify to match a patient with their appropriate therapy and, as Dr. Hsu mentioned, to tailor that in the setting of their other medical conditions.
JOHN WHYTE
So Dr. Hsu, it's all about precision medicine, it's all about personalized medicine, what do you do for my tumor type in my case? So I need to ask you, what's the role of comprehensive genomic testing, particularly when it comes to inoperable lung cancer? MELINDA HSU
I think that comprehensive genomic profiling is one of the main drivers for decision making in terms of how to treat inoperable lung cancer. Lung cancer patients are lucky in the sense that lung cancer is the poster child, I think, for precision medicine. There are so many different biomarkers now for patients with lung cancer that we have targeted therapies for. And so it's absolutely critical that every patient with inoperable lung cancer have this comprehensive genomic profiling done for their tumor. JOHN WHYTE
And I didn't ask you the question, Dr. Murray, because I knew what your answer was going to be. I have a different question for you coming from a center that focuses on it. There's a lot of data out there that shows that despite the fact that we think that cancer care is routinized, should be routinized, we know that a fairly large number of patients with cancer don't get this genomic testing. And sometimes, people will say, well, I just want to get started, I don't want to wait more time to start treatment. Help explain to our audience why it's so important. JOSEPH MURRAY
Absolutely. This has been a distinct challenge with the rise of comprehensive genomic profiling of cancers, not only in lung cancer, but it certainly remains a problem. Our data over the last couple of years suggests that less than half the patients are receiving complete comprehensive genomic profiling before initiation of their first therapy. And the way I describe this to patients is I don't want to just give them the first therapy I have available, I want to give them the best therapy that provides them ultimately the best outcomes over their life. And so my focus is on getting this testing done as efficiently as possible. And I use a combination of tissue and liquid biopsy testing to complete this comprehensive molecular profiling. I think that this can afford us avenues to increase the breadth and speed with which we can complete this testing for patients.
JOHN WHYTE
So Dr. Murray, why is this being done? Is it not readily available everywhere? Do some oncologists feel they don't need that information right now? Is it, as I said, the part of patients, they just want to get started? I mean, less than half is not a good percentage. JOSEPH MURRAY
Correct. It is all of the above. Part of this is education, not just on the fact of patient advocacy groups empowering patients to ask for this testing, but also to make sure the guidelines be right, which are rapidly expanding month on month with new indications and new genes to test. Expanding that education to an oncologist is really key as well. JOHN WHYTE
So there's certainly exciting innovations in genomic testing. And that's only going to get better. But where are we in terms of innovations in terms of treatments? Dr. Hsu, what excites you about what we might be seeing in the next, say, three to five years? MELINDA HSU
What excites me in the next three to five years for patients with inoperable lung cancer are the new treatments that I think will be available to them, not only different types potentially of immunotherapy or more targeted therapies for a broader number of genomic markers, but also treatments for our patients who've gotten that first line therapy and had a good response for several years, and then their cancer has gotten smarter than the treatments and figured out a way to mutate or continue to grow. And I think that that's an area where we need to focus really. And I think that there will be a lot of drugs in that setting for our patients who've kind of progressed on their first therapy. JOHN WHYTE
What do you say to a patient who's recently been diagnosed with inoperable lung cancer? What's your message to that person? JOSEPH MURRAY
My message is often quite clear. We can treat your cancer, although we cannot always cure it. And I do focus on the fact that treating the cancer is only one aspect. We must focus and treat the whole patient as well. And guiding a patient through the initial phases of that becomes absolutely critical. And identifying what barriers to effective therapy and what supportive therapies, including palliative care, that need to be integrated in a patient's care team becomes important. MELINDA HSU
The lung cancer is always treatable. And I think that we talk about what the goal of treatment really is because every patient has a different goal. And I'm an advocate for each patient's goal so that we can achieve that together. JOHN WHYTE
Doctors, I want to thank you for taking time today. MELINDA HSU
Thank you. JOSEPH MURRAY
Thanks so much for having us. [MUSIC PLAYING]