Slideshow: A Visual Guide to Understanding Osteoarthritis

Osteoarthritis: What Is It?
Also called "wear and tear" arthritis or degenerative joint disease, osteoarthritis (OA) is the progressive breakdown of the joints' natural shock absorbers. This can cause discomfort when you use the affected joints -- perhaps an ache when you bend at the hips or knees, or sore fingers when you type. Most people over 60 have some degree of OA, but it also affects people in their 20s and 30s.

Osteoarthritis: Symptoms
The symptoms of osteoarthritis tend to develop slowly. You may notice pain or soreness when you move certain joints or when you've been inactive for a prolonged period. The affected joints may also be stiff or creaky. Typically, osteoarthritis leads to morning stiffness that resolves in 30 minutes. When osteoarthritis affects the hands, some people develop bony enlargements in the fingers, which may or may not cause pain.
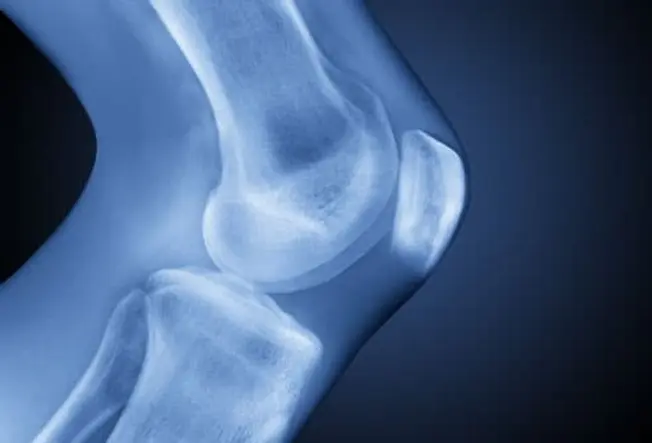
Osteoarthritis: Where Does It Hurt?
In most cases, osteoarthritis develops in the weight-bearing joints of the knees, hips, or spine. It's also common in the fingers. Other joints such as the elbow, wrist, and ankle are usually not affected, unless an injury is involved.

Osteoarthritis: What Causes It?
Every joint comes with a natural shock absorber in the form of cartilage. This firm, rubbery material cushions the ends of the bones and reduces friction in healthy joints. In general, as we age our joints become stiffer and cartilage can become more vulnerable to wear and tear. At the same time, repetitive use of the joints over the years irritates the cartilage. If it deteriorates enough, bone rubs against bone, causing pain and reducing range of motion.

Risk Factors You Can't Control
One of the major risk factors for osteoarthritis is something none of us can control -- getting older. Gender also plays a role. Over age 50, more women than men develop osteoarthritis. In most cases, the condition results from normal wear and tear over the years. But some people have a genetic defect or joint abnormality that makes them more vulnerable.

Risk Factors You Can Control
Because injured joints are more vulnerable to osteoarthritis, doing anything that damages the joints can raise your risk. This includes sports that have a high rate of injury and jobs that require repetitive motion, such as bending the knees to install flooring. Obesity is another risk factor -- it has been linked specifically to osteoarthritis of the hands, knees and hips.

Impact on Daily Life
Osteoarthritis affects each person differently. Some people have few symptoms despite the deterioration of their joints. Others experience pain and stiffness that may interfere with daily activities. If bony knobs develop in the small joints of the fingers, tasks such as buttoning a shirt can become difficult. Osteoarthritis of the knees or hips can lead to a limp. And osteoarthritis of the spine can cause debilitating pain and/or numbness.

Diagnosing Osteoarthritis
To help your doctor make an accurate diagnosis, you'll need to describe your symptoms in detail, including the location and frequency of any pain. Your doctor will examine the affected joints and may order X-rays or other imaging studies to see how much damage there is, and to rule out other joint conditions. Your doctor may suggest doing blood tests to rule out other forms of arthritis.

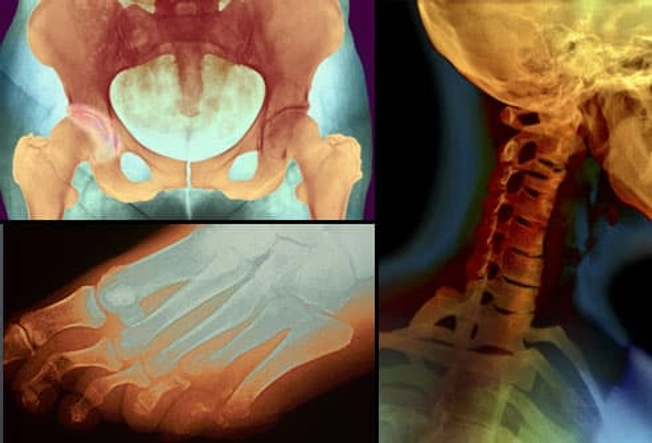
Long-Term Complications
Unlike rheumatoid arthritis, osteoarthritis does not affect the body's organs or cause illness. But it can lead to deformities that take a toll on mobility. Severe loss of cartilage in the knee joints can cause the knees to curve out, creating a bow-legged appearance (shown on the left). Bony spurs along the spine (shown on the right) can irritate nerves, leading to pain, numbness, or tingling in some parts of the body.

Treatment: Physical Therapy
There is no treatment to stop the erosion of cartilage in the joints, but there are ways to improve joint function. One of these is physical therapy to increase flexibility and strengthen the muscles around the affected joints. The therapist may also apply heat or cold therapies such as heat packs or compresses to relieve pain.

Supportive Devices
Supportive devices, such as finger splints or knee braces, can reduce stress on the joints and ease pain. If walking is difficult, canes, crutches, or walkers may be helpful. People with osteoarthritis of the spine may benefit from switching to a firmer mattress and wearing a back brace or neck collar.

Medication for OA
When osteoarthritis flares up, many patients find relief with over-the-counter pain and anti-inflammatory medication, such as aspirin, ibuprofen, or acetaminophen. Pain-relieving creams or sprays can also help when applied directly to the sore area. If pain persists despite the use of pills or creams, your doctor may suggest an injection of steroids or hyaluronans directly into the knee joint.
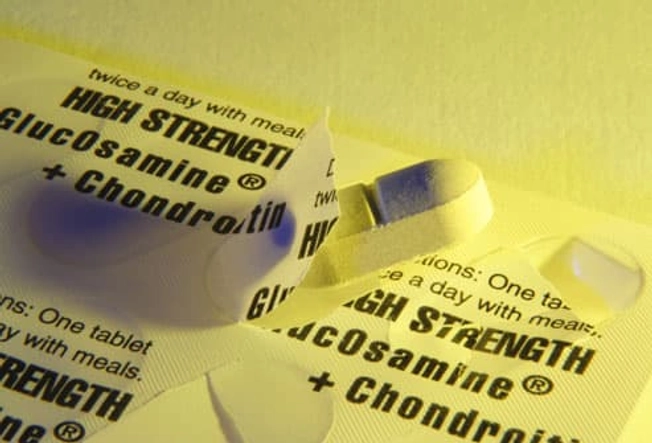
Supplements
Overall studies suggest no benefits of glucosamine and chondroitin -- supplements available at pharmacies and health food stores touted for relieving pain and stiffness for people with osteoarthritis. Check with your doctor before using chondroitin, especially if you take blood-thinners. Other supplements such as antioxidants vitamin C and E and vitamin D have not been shown to help.

Osteoarthritis and Weight
If you're overweight, one of the most effective ways to relieve pain and improve function of joints in the knee or hip joints is to shed a few pounds. Even modest weight loss has been shown to reduce symptoms of osteoarthritis by easing the strain on weight-bearing joints. Losing weight not only cuts down on pain, but may also reduce long-term joint damage.

Osteoarthritis and Exercise
People with osteoarthritis may avoid exercise out of concern that it will cause pain. But low-impact activities such as swimming, walking, or bicycling can improve mobility and increase strength. Training with light weights can help by strengthening the muscles that surround your joints. For example, strengthening the quadriceps can reduce pain in the knees. Ask your doctor or physical therapist which exercises are best for you.
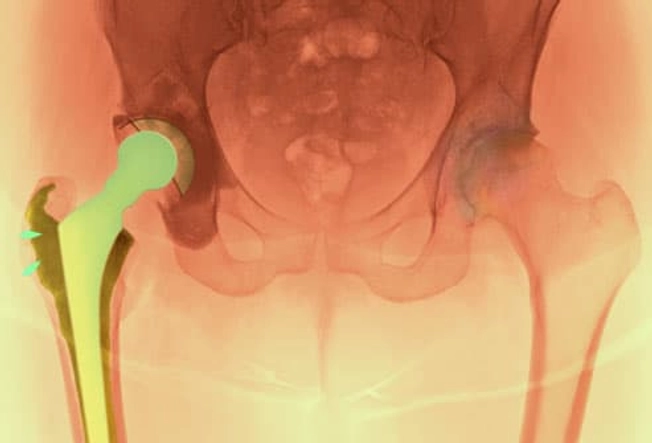
Is Surgery for You?
If osteoarthritis interferes significantly with everyday life and the symptoms don't improve with physical therapy or medication, surgery is an option. Joint replacement or resurfacing is used on those with severe OA . The knee and hip are the joints that are replaced most often.
Preventing Osteoarthritis
The most important thing you can do to ward off osteoarthritis is keep your weight in check. Over the years, extra weight puts stress on the joints and may even alter the normal joint structure. Preventing injuries is also important. Take precautions to avoid repetitive motion injuries on the job. If you play a sport, use proper equipment and observe safety guidelines.