Asthma and allergies often go hand-in-hand. Asthma is a disease of the branches of the windpipe (bronchial tubes), which carry air in and out of the lungs. There are several different types of asthma.
Allergic asthma is a type of asthma that is triggered by an allergy (for example, pollen or mold spores). According to the American Academy of Allergy, Asthma and Immunology, many of the 25 million Americans with asthma also have allergies, and this is called allergic asthma.
Air is normally taken into the body through the nose and windpipe and into the bronchial tubes. At the end of the tubes are tiny air sacs called alveoli that deliver fresh air (oxygen) to the blood. The air sacs also collect stale air (carbon dioxide), which is exhaled out of the body. During normal breathing, the bands of muscle surrounding the airways are relaxed and air moves freely. But during an asthma episode or "attack," there are three main changes that stop air from moving freely into the airways:
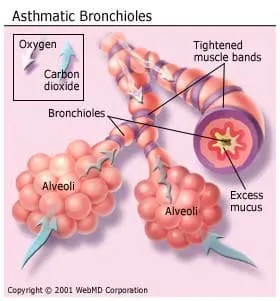
- The bands of muscle that surround the airways tighten, causing them to narrow in what is called "bronchospasm."
- The lining of the airways becomes swollen, or inflamed.
- The cells that line the airways produce more mucus, which is thicker than normal.
The narrowed airway makes it more difficult for air to move in and out of the lungs. As a result, people with asthma feel they cannot get enough air. All of these changes make breathing difficult.
What Are the Most Common Symptoms of Asthma?
Symptoms of asthma strike when the airways undergo the three changes described above. Some people can go a long time between asthma episodes while others have some symptoms every day. Common symptoms of asthma include:
- Frequent cough, especially at night
- Shortness of breath
- Wheezing
- Chest tightness, pain, or pressure
Not every person with asthma has the same symptoms in the same way. You may not have all of these asthma symptoms, or you may have different symptoms at different times. Your symptoms may also vary from one asthma episode to the next. Symptoms may be mild during one asthma episode and severe during another.
Mild asthma episodes are generally more common. Usually, the airways open up within a few minutes to a few hours. Severe episodes are less common, but last longer and require immediate medical help. It is important to recognize and treat even mild symptoms to help prevent severe episodes and keep asthma in control.
If you suffer from allergies and asthma, a reaction to any offending allergy-causing substance can worsen asthma symptoms.
What Are the Early Warning Signs of an Asthma Attack?
Early warning signs start before the more prominent symptoms of asthma and are the earliest signs that a person's asthma is worsening. Early warning signs and symptoms of an asthma attack include:
- Frequent cough, especially at night
- Losing your breath easily or shortness of breath
- Feeling very tired or weak when exercising, in addition to wheezing, coughing, or shortness of breath
- Decreases or changes in peak expiratory flow, a measurement of how fast air comes out of the lungs when you exhale forcefully
- Signs of a cold or other upper respiratory infections, or allergies
- Difficulty sleeping
If you have any of these asthma symptoms, seek treatment as soon as possible to prevent experiencing a severe asthma attack.
Who Gets Asthma?
Anyone can get asthma, although it tends to run in families. An estimated 25 million adults and children in the U.S. have asthma. The disease is becoming more widespread.
What Causes Asthma?
Asthma is a problem in the airways due to multiple factors. The airways in a person with asthma are very sensitive and react to many things, which are referred to as "triggers." Coming into contact with these triggers often produces asthma symptoms.
There are many kinds of asthma triggers. Reactions are different for each person and vary from time to time. Some people have many triggers while others have none that they can identify. One of the most important aspects of asthma control is avoiding triggers when possible.
Common asthma triggers include:
- Infections: colds, flu, sinus infections
- Exercise: very common in children*
- Weather: cold air, changes in temperature
- Tobacco smoke and air pollution
- Allergens: substances that cause allergic reactions in the lungs, including dust mites, pollens, pets, mold spores, foods, and cockroaches
- Dust or items causing dust
- Strong odors from chemical products
- Strong emotions: anxiety, and crying, yelling, or laughing hard
- Medicines: aspirin, ibuprofen, and beta blocker drugs used to treat conditions including high blood pressure, migraines, or glaucoma
*Note: While exertion may be an asthma trigger, exercise should not be avoided. With a good treatment plan, children (and adults) can exercise as long and as much as desired, except during an asthma attack.
How Is Asthma Diagnosed?
Doctors can use a number of tests to diagnose asthma. First, the doctor reviews your medical history, symptoms, and does a physical exam. Next, tests may be given to check the general condition of your lungs, including:
- Chest X-ray in which a picture of the lungs is taken.
- Pulmonary function test (spirometry): A test that measures how well the lungs can take in air and how well this air can be exhaled (lung function). The patient blows into a tube placed between the lips.
- Peak expiratory flow: A test that measures the maximum speed that air can be exhaled from the lungs. The patient blows into a hand-held device called a peak flow meter.
- Methacholine challenge test: A test used to see if the airways are sensitive to methacholine, an irritant that tightens the airways.
- Other tests, such as allergy tests, blood tests, sinus X-rays and other imaging scans, and esophageal (throat) pH tests may also be ordered. These tests can help your doctor find out if other conditions are affecting your asthma symptoms.
What Is the Treatment for Asthma?
By avoiding asthma triggers, taking medication, and carefully monitoring daily asthma symptoms, asthma attacks can be avoided or at least limited. Proper use of medication is the basis of good asthma control. Drugs used to treat asthma include bronchodilators, anti-inflammatories, leukotriene modifiers and immunomodulators.
Bronchodilators to Treat Asthma
These drugs treat asthma by relaxing the muscle bands that tighten around the airways. They rapidly open the airways, letting more air in and out of the lungs and improving breathing.
Bronchodilators also help clear mucus from the lungs. As the airways open, the mucus moves more freely and can be coughed out more easily. In the short-acting form, bronchodilators relieve or stop asthma symptoms and are very helpful during an asthma attack. The three main types of bronchodilators are beta2 agonists, anticholinergics, and theophylline.
Anti-inflammatories and Asthma
These asthma drugs, which include inhaled corticosteroids such as Alvesco, Arnuity Ellipta, Asmanex, Azmacort, Flovent, Qvar, and Pulmicort, reduce swelling and mucus production in the airways. As a result, airways are less sensitive and less likely to react to triggers. Anti-inflammatories are taken daily for several weeks before they begin to control asthma. These asthma drugs also lead to fewer symptoms, better airflow, less sensitive airways, less airway damage, and fewer asthma episodes. If taken every day, they can control or prevent asthma symptoms.
Another type of anti-inflammatory asthma drug is cromolyn sodium. This medication is a mast cell stabilizer, which means that it helps prevent the release of asthma-inducing chemicals from cells in the body known as mast cells. Intal is a drug commonly used in children and for exercise-induced asthma.
Leukotriene Modifiers for Asthma Treatment
Leukotriene modifiers used for asthma treatment include the drugs Accolate, Singulair, and Zyflo. Leukotrienes are chemicals that occur naturally in our bodies and cause tightening of airway muscles and production of mucus and fluid. Leukotriene modifiers work by limiting these reactions, improving airflow and reducing asthma symptoms. They are taken as pills (or as oral granules that can be mixed with food) one or two times a day and decrease the need for other asthma medications. The most common side effects are headache and nausea. Leukotriene modifiers may interact with other drugs, like Coumadin and theophylline. Inform your doctor about any medications you are taking.
Immunomodulators and Asthma
The drug Omalizumab (Xolair) is an antibody that blocks immunoglobulin E (IgE). This prevents an allergen from triggering an asthma attack. Xolair is given as an injection. In order to receive this therapy a person has to have an elevated IgE level and have known allergies. The allergies need to be confirmed by either blood or skin test.
Reslizumab (Cinqair) is a maintenance medication for those with severe asthma. It would be used along with your regular asthma medicines. It is given every four weeks as an intravenous injection. This medicine works by reducing the number of a specific type of white blood cells, called eosinophils that play a role in causing asthma symptoms. It can reduce severe asthma attacks. Reslizumab can be used by those age 18 and older.
Mepolizumab (Nucala) also targets the levels of blood eosinophils. It is given as an injection every 4 weeks and is used as a maintenance therapy medication.
How Are Asthma Drugs Taken?
Many asthma drugs are taken using a device called a "hydrofluoroalkane inhaler" or HFA Inhaler (formerly called a metered dose inhaler,) a small aerosol canister in a plastic container that releases a burst of medication when pressed down from the top.
Several asthma drugs can also be taken as a powder inhaled through the mouth from a device called a dry powder inhaler. Asthma drugs can also be taken as vapors, pills, liquids, shots or intravenously.
What Else Should I Do to Help Control My Asthma?
To control asthma, it's also important to keep track of how well lungs are functioning. Asthma symptoms are monitored using a peak flow meter -- a device that measures the speed of air that coming out of the lungs when you exhale forcefully. This measurement is called peak expiratory flow (PEF) and is calculated in liters per minute.
The meter can alert you to changes in the airways that may be a sign of worsening asthma before you have symptoms. By taking daily peak flow readings you can learn when to adjust medications to keep asthma under control. Your doctor can also use this information to adjust your treatment plan.
Can Asthma Be Cured?
There's no cure for asthma, but it can be treated and controlled. In most cases, people with asthma can live free of symptoms by following their treatment plan.

