How Do I Know If I Have Endometrial Cancer?
If women have symptoms of endometrial cancer, their doctor will examine them and possibly order blood and urine tests.
Other possible tests include:
Pelvic exam and Pap smears, which look for cervical cancer, can also find a small number of endometrial cancers before symptoms develop.
Transvaginal ultrasound, in which the doctor inserts a wand-like instrument into the vagina. The instrument aims high-frequency sound waves at the uterus. The pattern of the echoes they produce creates a picture. Saltwater can be placed into the uterus through the cervix before the ultrasound test to give a clearer picture. This is called a sonohysterogram. If the endometrium looks too thick or irregular, the doctor can perform an endometrial biopsy in the office or a dilation and curettage (D&C) in the operating room.
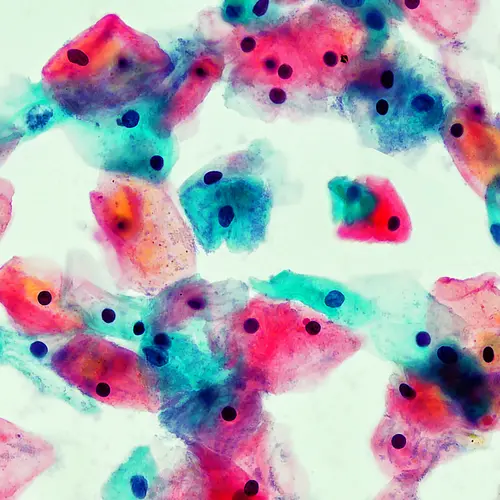
The definitive test is a biopsy (taking and testing a tissue sample from the uterus). If a biopsy confirms the diagnosis, the doctor will order imaging tests such as a CT scan or MRI; blood tests for CA-125, a marker seen both with ovarian and endometrial cancer; and a colonoscopy. The doctor may also order exploratory surgery (opening the abdomen) to determine how far the disease has spread.
What Are the Treatments for Endometrial Cancer?
Surgery is the standard treatment for endometrial cancer that has not spread. It is also an effective prevention for women at high risk of developing the disease. The most successful treatment for early cancer is total hysterectomy with bilateral salpingo-oophorectomy, in which the uterus, cervix, ovaries, and fallopian tubes are removed. In addition, any suspicious lymph nodes and other tissue and organs are biopsied and also may be removed. This surgery is most likely to prevent the cancer from coming back.
If the cancer has spread beyond the uterus, then after surgery the patient is given radiation, often in combination with chemotherapy, to wipe out the remaining cancer cells. Some doctors also recommend radiation when the tumor is large but has not spread beyond the uterus.
Patients with widespread endometrial cancer usually receive hormone therapy, usually progesterone, to slow the cancer's growth. Chemotherapy or radiation might also be given to reduce the size and number of tumors -- all of which can prolong life and relieve symptoms. If treatment successfully destroys distant tumors and the remaining cancer is confined to the uterus, cervix, ovaries, and fallopian tubes, surgery may also be performed.
Patients in remission need checkups every few months for several years. If cancer comes back, it usually happens within three years. Caught early, cancer that comes back may be cured with aggressive radiation, chemotherapy, or more surgery.
To help cope with the emotional difficulties of having uterine cancer, patients might consider joining a support group. Counseling may also be helpful.