What Is Polycythemia Vera?
Polycythemia vera (PV) is a blood cancer that begins in the marrow of your bones, the soft center where new blood cells grow. It causes your marrow to make too many red blood cells so your blood is too thick. You may be more likely to have clots, a stroke, or a heart attack.
This disease gets worse slowly, usually over many years. It can be life-threatening if you don't get treatment, but the right care can help you live a long life.
Most people who have PV don’t get diagnosed until they’re 60 or older, usually after a routine blood test. But it can happen at any age. Men get it more often than women.
It's common to worry when you find out that you have cancer. Remember that everyone is different and that all cancers aren’t the same. With the support of your doctor, family, friends, and other people who have polycythemia vera, you’ll be in the best position to manage it.
Polycythemia Vera Causes
Your bone marrow makes three types of blood cells:
- Red
- White
- Platelets
Red blood cells carry oxygen, white ones fight infections, and platelets clot your blood to stop bleeding.
Most people with polycythemia vera have too many red blood cells. But it can also cause you to have too many white blood cells and platelets.
PV is caused by a gene (either JAK2 or TET2) that doesn’t work the way it should. Most likely, the problem happened over the course of your life. Rarely, parents can pass these faulty genes to children.
Polycythemia Vera Symptoms
At first, you may not notice any problems. When they do show up, polycythemia vera symptoms can include:
- Headaches
- Double vision
- Dark or blind spots in your vision that come and go
- Itching all over your body, especially after you've been in warm or hot water
- Sweating, especially at night
- A red face that looks like sunburn or blushing
- Weakness
- Dizziness
- Weight loss
- Shortness of breath
- Tingling or burning in your hands or feet
- Painful joint swelling
You may also feel pressure or fullness below your ribs on your left side. This might mean PV has enlarged your spleen, an organ that helps filter your blood.
Polycythemia Vera Complications
Blood clots can cause a heart attack, a stroke, or deep vein thrombosis (DVT). They might also make your liver or spleen larger. If your organs don’t get enough blood, you could have chest pain or heart failure.
Having too many red blood cells might cause stomach ulcers, gout, or kidney stones.
PV can also lead to more serious blood diseases like acute leukemia or myelofibrosis. Acute leukemia is a blood cancer that gets worse quickly. Myelofibrosis is a condition in which your bone marrow fills with scar tissue.
Polycythemia Vera Diagnosis
Your doctor will start with a physical exam, including a check of your spleen. They’ll ask about your symptoms and see if your face is unusually red.
You may have some blood tests, including:
- Complete blood count(CBC). Your doctor takes a sample of your blood and sends it to a lab, where a machine counts the number of red blood cells, white blood cells, and platelets. An unusually high number of any of these could be a sign of polycythemia vera.
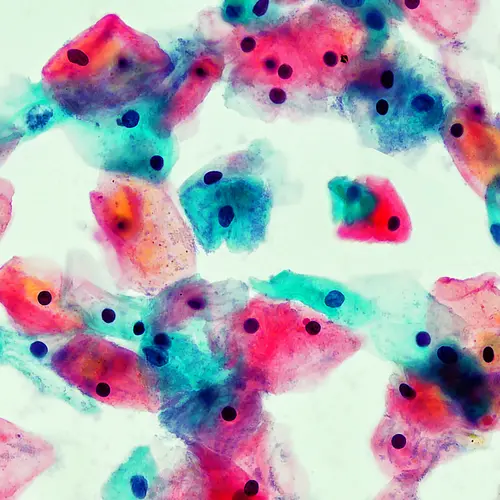
- Blood smear. Your doctor looks at a sample of your blood through a microscope. It's a way to check for other diseases that are sometimes linked to PV.
- EPO level. This test measures how much of the hormone EPO is in your blood. EPO tells your bone marrow to make blood cells. People who have polycythemia vera have very low amounts of it.
You may also need a bone marrow biopsy. The results can show your doctor if your bone marrow makes too many blood cells.
For this test, your doctor will take samples of your marrow, usually from the back of your hip bone.
You lie down on a table and get a shot that will numb the area. Then, your doctor uses a needle to take out a small amount of bone marrow. It's an outpatient procedure, which means you don't have to stay overnight in a hospital. You can get it done in a clinic, a hospital, or your doctor's office.
Questions for your doctor
Before your appointment, it's a good idea to make a list of things to ask your doctor, such as:
- Which treatment do you recommend?
- What are the side effects?
- How can I prevent complications?
- Since I have polycythemia vera, am I more likely to have a stroke or heart attack?
- How can I ease my symptoms?
Polycythemia Vera Treatment
If you don't have many symptoms, you might not need treatment for PV right away. Your doctor will keep a close watch on you.
If you do need treatment, it will be aimed at lowering the amount of red blood cells your body makes and preventing blood clots and other complications.
Your options include:
Phlebotomy. This is often the first treatment for people who have polycythemia vera.
Your doctor takes blood from your vein so you have fewer blood cells. It's a lot like donating blood. After it's done, your blood will be thinner, and it’ll flow more easily. You'll usually feel better, too. Some symptoms will ease, like headaches or dizziness.
Your doctor will decide how often you need phlebotomy. Some people with PV don’t need any other treatment for many years.
Low-dose aspirin. This keeps platelets from sticking together. That makes you less likely to get blood clots, which in turn makes heart attacks or strokes less likely. Most people with polycythemia vera take low-dose aspirin.
Medicine to lower blood cells. If you need more help, your doctor may prescribe hydroxyurea (Droxia, Hydrea), a pill that lowers your red blood count and eases symptoms.
Other drugs like interferon alfa (Intron A) or ropeginterferon alfa-2b-njft (Besremi) help your immune system cut back on making blood cells. You might take busulfan (Busulfex, Myleran) or ruxolitinib (Jakafi) if hydroxyurea isn’t helpful or if it causes severe side effects.
If you have itching that doesn't go away, your doctor may give you antihistamines.
Lifestyle Changes
Keep yourself comfortable and as healthy as possible during treatment:
- Don't smoke or chew tobacco. Tobacco narrows blood vessels, which can make blood clots more likely.
- Get light exercise, such as walking, to help your circulation and keep your heart healthy.
- Do leg and ankle exercises to keep clots from forming in the veins of your legs. Your doctor or a physical therapist can show you how.
- Bathe or shower in cool water if warm water makes you itch.
- Keep your skin moist with lotion, and try not to scratch.
Polycythemia Vera Prognosis
There's no cure, but the right treatment can help you manage this disease for many years.
Talk to your friends and family about what you’re dealing with. You may also want to join a support group for people who’ve been in your position.
The MPN Research Foundation has more information about polycythemia vera. It can also help you find support groups.