Prostate cancer is not often a cause of erectile dysfunction (or ED). However, treatments for the disease can cause it. The current methods of treating prostate cancer, including surgery with radical prostatectomy (removal of the entire prostate gland), radiation therapy -- whether by external beam or brachytherapy (seed implant) -- and hormone therapy, can all cause ED.
When Can Erectile Dysfunction Occur After Prostate Cancer Treatment?
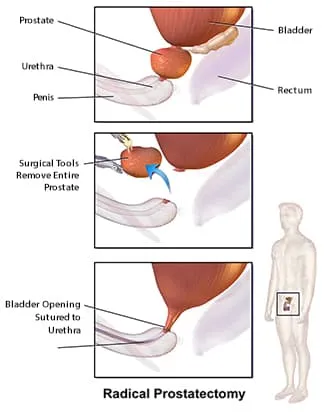
- Radical prostatectomy.Erectile dysfunction can begin immediately following the removal of the entire prostate and surrounding tissues, whether the nerve-sparing or non-nerve-sparing technique is used. If the nerve-sparing technique is used, recovery from ED may occur within the first year following the procedure. Recovery of erectile function after a non-nerve-sparing technique is unlikely but possible.
- Radiation therapy. The onset of ED following radiation therapy is gradual and usually begins within 2 to 3 years following treatment. Without treatment for erectile dysfunction, ED is usually permanent.
- Hormone therapy. When hormone therapy is used, ED may occur approximately two to four weeks following the initiation of the therapy and is usually accompanied by a decreased desire for sex. Without treatment, the ED may become permanent.
How Is Erectile Dysfunction Treated Following Prostate Cancer Treatment?
The current treatment options for erectile dysfunction for people who have received treatment for prostate cancer include:
- Pills, including Cialis, Levitra, Stendra, Staxyn, and Viagra
- Intracavernous injection therapy
- Vacuum constriction device
- Intraurethral therapy
- Penile prosthesis
Talk to your doctor or a specialist regarding treatment options for ED.

