Slideshow: A Visual Guide to IBD

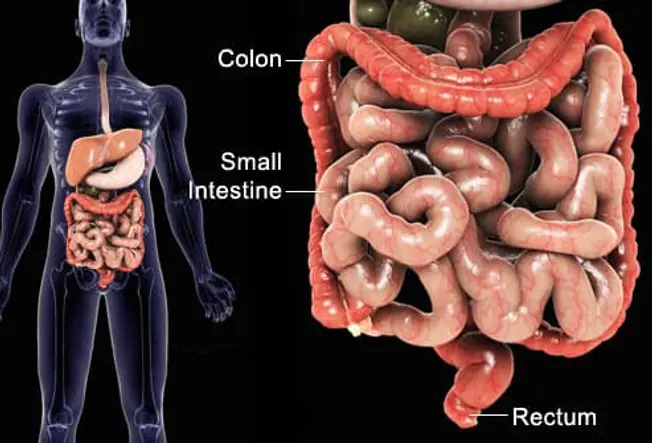
What Is Inflammatory Bowel Disease?
Inflammatory bowel disease (IBD) refers to chronic conditions that cause inflammation in some part of the intestines. The intestinal walls become swollen, inflamed, and develop ulcers, which can cause discomfort and serious digestive problems. The exact symptoms depend on which part of the digestive tract is involved.

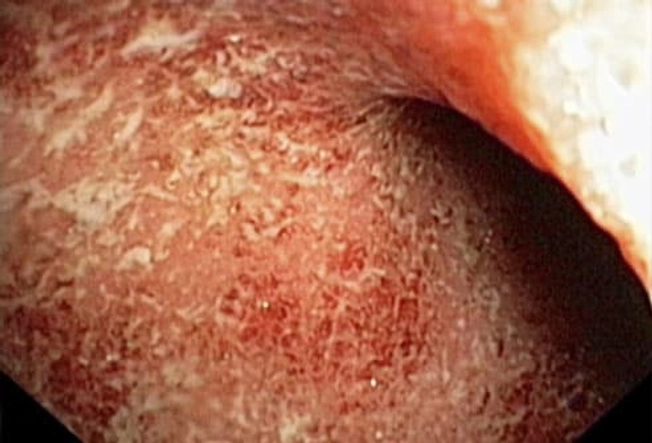
Types of IBD: Crohn's Disease
Crohn's disease is a form of IBD that can happen anywhere along the digestive tract -- from the mouth to the anus. It affects the deeper layers of the digestive lining and can show up as "skip lesions" between healthy areas. Crohn's often involves the small intestine, the colon, or both. Internal tissues may develop shallow, crater-like areas or deeper sores and a cobblestone pattern, as seen here.
Types of IBD: Ulcerative Colitis
Unlike Crohn's disease, ulcerative colitis involves only the colon and rectum. Inflammation and ulcers usually affect only the lining in these areas, compared with the deeper lesions seen in Crohn's disease. Often only the lower (sigmoid) colon is affected, but it can happen higher up, too. The more of the colon that is affected, the worse the symptoms will be.

Symptoms of IBD
The symptoms of ulcerative colitis and Crohn's disease are similar:
- Abdominal pain or cramping
- Diarrhea more than once a day
- Bloody stools
- Weight loss

Other Symptoms
People with IBD may have symptoms outside the digestive tract, such as:
- Mouth sores and skin problems
- Arthritis
- Eye problems that affect vision

What's the Cause?
Doctors aren't sure why some people get IBD. Most believe something triggers the body's immune system to produce an unhealthy inflammatory reaction in the digestive tract. Researchers have found specific genes linked to ulcerative colitis and Crohn's disease.

Who Gets it?
IBD strikes men and women equally. It most often begins during the teenage years or early adulthood, but can develop at other times, too. People with a family history of IBD are at least 10 times more likely to develop the condition than those with no history. Caucasians and people of Jewish descent also have an increased risk.

IBD Is Not IBS
IBD is sometimes confused with IBS, which stands for irritable bowel syndrome. Both conditions can cause chronic digestive problems, but there are key differences between the two. People with IBD have inflammation, ulcers, and other damage visible inside the digestive tract. In contrast, there is no damage in IBS, despite symptoms such as cramping, diarrhea, and constipation. IBS is much more common but less serious than IBD.
Conditions That Mimic IBD
There are other digestive disorders that may first be mistaken for IBD. The symptoms of diverticulitis are belly pain, bloating, and diarrhea -- much like IBD. But this condition involves inflamed or infected pouches along the colon wall. Another example is celiac disease, which causes cramping and frequent diarrhea, but the trigger is a protein in food called gluten. Testing can help doctors know if it’s really IBD..
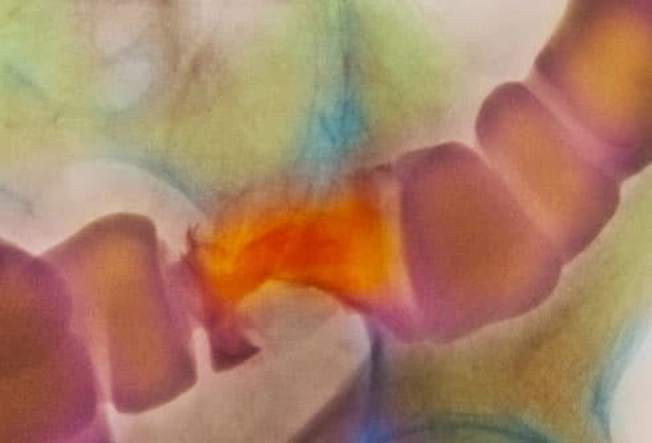
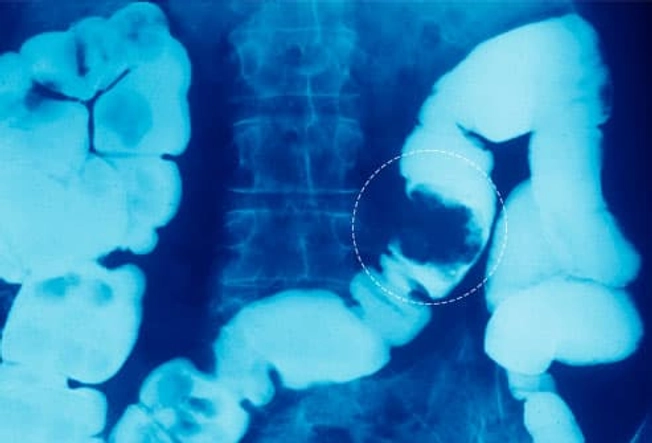
Barium X-ray
Several tests can help diagnose IBD. One that's sometimes done is a barium X-ray. Barium is a chalky fluid that you may take by mouth or as an enema. As it flows through the intestines, barium shows up on the X-ray. This helps doctors spot problem areas, such as ulcers, swelling, narrowing (seen here), or intestinal blockages. If problems show up, your doctor may ask you to get more imaging, such as a CT scan.

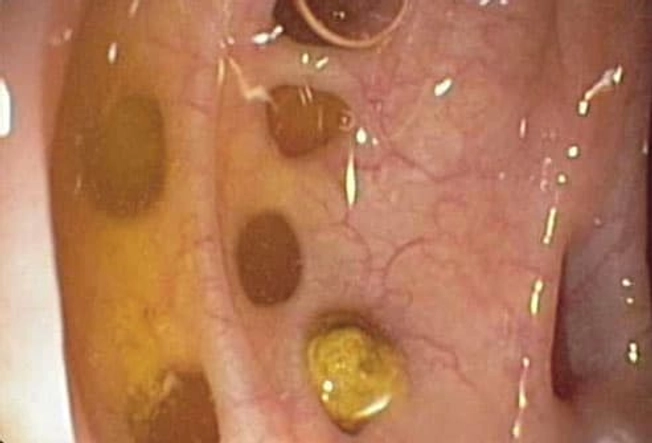
Colonoscopy
This is the most important test for diagnosing IBD. This procedure uses a thin tube with a camera to give doctors a direct view of the inside of the colon. Even small ulcers and mild inflammation can be seen this way. If any areas look unusual, the doctor may take a tissue sample (biopsy) for further investigation. Other tests for IBD include blood work to look for signs of inflammation or infection.

Choosing a Doctor for IBD
Doctors who specialize in treating people with digestive disorders are called gastroenterologists. Ask your regular doctor for referrals. You may also want to ask if there are clinical trials in your area. Clinical trials offer the possibility of trying new treatments that are not yet on the market.

What to Expect
The symptoms of IBD range from mild to severe and may come and go over time. Most people have flare-ups followed by long periods without symptoms. This is called remission, and it can last for months or even years. In ulcerative colitis, about 5% to 10% of people have symptoms all the time. Chronic belly pain and urgent trips to the bathroom can interfere with work, child care, and social life.

What Stress Does
Although stress doesn’t cause IBD, some people report that their symptoms get worse in times of stress. So when you’re under pressure, you may want to notice whether it affects your IBD or brings on a flare if you’ve been in remission.
Complications: Obstruction
In Crohn's disease, chronic inflammation can make the inside of the intestine so narrow that nothing can pass through. Doctors call this “bowel obstruction.” It causes digesting food and gas to get stuck in the digestive tract. The symptoms include severe cramping, nausea, vomiting, and a swollen belly. Bowel obstructions are treated in the hospital. If the obstruction does not clear on its own, you may need surgery.
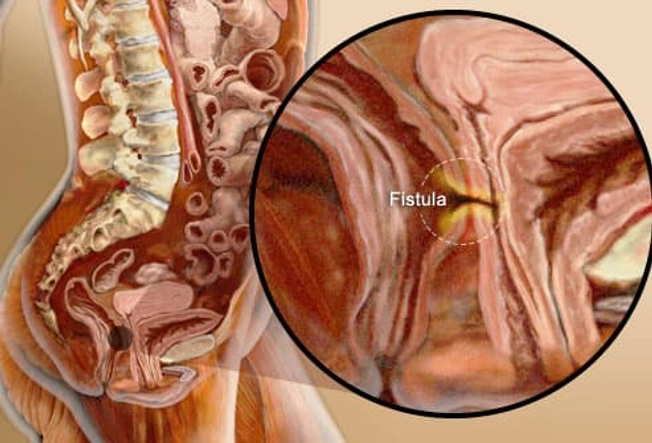
Complications: Abscess or Fistula
Deep ulcers sometimes create a pocket of pus, called an abscess. Symptoms include fever, pain, and swelling. If an ulcer breaks through to a nearby organ, it creates a tunnel called a fistula. A fistula between the colon and the vagina can allow bacteria into the vagina. A fistula to the bladder can cause chronic urinary tract infections. One that reaches the skin can create external sores. Fistulas and some abscesses are often treated with surgery.

Does IBD Cause Colon Cancer?
Most people with IBD don't get colon cancer. But those who have had IBD for at least 8 years have a higher risk of developing colon cancer. The risk is even greater when inflammation affects the entire colon. Ask your doctor about regular screening -- colorectal cancer is easiest to treat when it is found early

Foods to Watch
Food doesn't cause this disease, but specific items can make your symptoms worse. These trigger foods are different for each person, but some common culprits are alcohol, coffee, soda, spicy foods, beans, fatty foods, high-fiber foods, nuts and seeds, raw fruits and vegetables, red meat, and dairy products (if you're lactose intolerant).

Low-Residue Diet
If Crohn's disease has caused a narrowing of your small intestine, your doctor may recommend a low-residue diet. This means avoiding foods that add bulk to the stool, including nuts, seeds, raw fruits, and raw vegetables. Usually diet changes are temporary. This diet may help cut belly pain, cramping, and diarrhea, although more research is needed.

Nutritional Needs
When Crohn's disease attacks the small intestine, the body may not be able to absorb all the nutrients it needs. Poor absorption plus poor appetite can lead to malnutrition. To avoid this, try to eat a well-balanced diet with smaller meals more often throughout the day -- and drink enough fluids to stay hydrated. A registered dietitian can help. Your doctor may recommend vitamin and mineral supplements, too.

Lower Your Stress
Learning stress management techniques may help you handle IBD. Yoga, meditation, and exercise can all be beneficial. Talk therapy or group therapy can also be good ways to manage the emotional side of the condition.

Medications
In mild to moderate cases of IBD, treatment usually starts with medications called aminosalicylates. These are anti-inflammatory drugs that can help treat IBD and keep it in remission. During a flare, your doctor may also prescribe corticosteroids to reduce inflammation and help you reach remission. Other meds for more severe IBD aim to stop the immune system from causing inflammation. These include “immunomodulators” and “biologics.”

Combination Therapy
Getting an immunomodulator and a biologic may work best for people with moderate to severe Crohn's disease. Immunomodulators make your immune system less active. Biologics, which you get by injection, block the action of proteins that are key in the immune response that causes inflammation

Surgery
When IBD causes severe damage to the colon, it may need to be surgically removed. This can cure ulcerative colitis, because the condition only affects the colon. Surgery usually cannot cure Crohn's disease, because symptoms can continue in other parts of the digestive tract. Thanks to surgical advances, most people who have their colons removed will be able to have normal bowel movements without an ostomy bag.

Exercise and IBD
Doctors may recommend light exercises for people with IBD. This includes activities like yoga, tai chi, or walking, which don't involve a lot of jarring that could make digestive symptoms worse. Regular exercise may aid digestion. It can also help you feel better and less stressed, which may keep symptoms in check.

Living Better with IBD
IBD may be a lifelong condition, but there are ways to keep it in check. Through medications, lifestyle changes, and stress management, many people with IBD can still do the things they want to do. If IBD hampers your daily life, tell your doctor.