What Is Gum Disease?
Gums are the tissues that surround your teeth and hold them in place. Gum disease is an infection of this tissue. Your dentist might call it periodontal disease or periodontitis.
Gum disease starts when bacteria grow in your mouth. Bacteria build up when you don’t brush your teeth or floss well enough. Without treatment, gum disease can cause swelling, redness, pain, and tooth loss.
Almost half of adults ages 30 and older have signs of gum disease. About 9% of adults have severe gum disease.
Gingivitis vs. Periodontitis
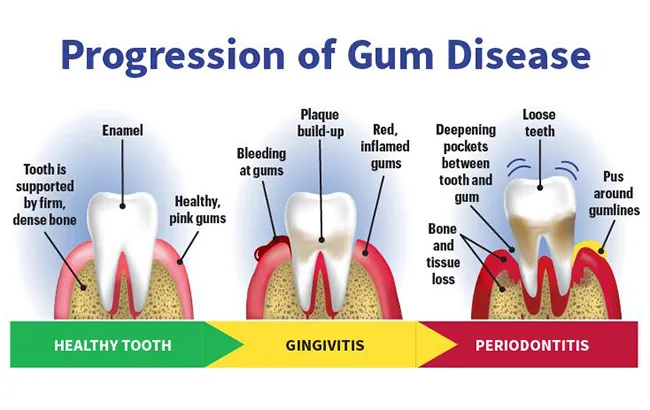
Gingivitis is swelling, redness, and bleeding in the part of your gums that surround your teeth. It's a milder form of gum disease that can lead to periodontitis if you don't treat it.
When you forget to brush, floss, and rinse with mouthwash, a sticky film of bacteria and food called plaque builds up around your teeth. The gunk releases acids that attack your teeth’s outer shell, called enamel, and cause decay. After 72 hours, plaque hardens into tartar, which forms along the gumline and makes it hard to clean your teeth and gums completely. Over time, this buildup irritates and inflames your gums, causing gingivitis.
If you have periodontitis, the inner layer of the gum and bone pull away from the teeth and form pockets. These small spaces between the teeth and gums collect debris and can become infected. The body's immune system fights the bacteria as the plaque spreads and grows below the gumline.
Toxins or poisons – produced by the bacteria in plaque as well as the body's "good" enzymes involved in fighting infections – start to break down the bone and connective tissue that hold teeth in place. As the disease gets worse, the pockets deepen and more gum tissue and bone are destroyed. When this happens, teeth are no longer anchored in place, they become loose, and tooth loss occurs. Gum disease is the leading cause of tooth loss in adults.
You can prevent or reverse gingivitis if you brush your teeth, floss, and have regular dental cleanings and checkups.
Periodontal Disease Stages
Periodontal disease has four stages. It starts with mild swelling and redness of the gums and can lead to bone damage and tooth loss.
Gingivitis
At this early stage of periodontal disease, your gums may be red and swollen. They might bleed when you brush your teeth. But your bones are still in place. You can reverse gum disease at this stage.
Mild periodontitis
Now the bacteria have gotten underneath your gums and reached your bones. Your gums might pull away from your teeth and create pockets. Plaque and bacteria fill those pockets and damage your teeth even more.
Moderate periodontitis
Bacteria eat away at the gum and bone that hold your teeth in place. Your gums might hurt. You may see pus around your gumline, which is a sign of infection.
Advanced periodontitis
The bone and tissue around your teeth are more damaged. In time, your teeth may get loose and fall out.
Gum Disease Causes
Plaque is the main cause of gum disease. Gingivitis happens like this:
- Bacteria collect on your teeth after you eat sweet or starchy foods.
- If you don't brush and floss well, those bacteria form a sticky film called plaque on your teeth.
- Plaque turns into a hard deposit called tartar along your gums.
- Tartar traps bacteria on your teeth. The bacteria cause even more tooth damage.
- Your gums get irritated, red, and swollen. They may bleed when you brush your teeth.
After you've had gingivitis for a while, your gums may pull away from your teeth and form pockets. These small spaces can fill with bacteria, plaque, and tartar and become infected.
The infection breaks down the bone and connective tissue that hold your teeth in place. After a while, your teeth may get loose enough to fall out. Gum disease is the most common cause of tooth loss in adults.
Things like these increase your risk of gum disease:
- Hormone changes during pregnancy, puberty, menopause, and periods leave gums more sensitive, and make it easier for gingivitis to develop.
- Diseases like cancer, HIV, and diabetes increase the risk of infections, including periodontal disease.
- Some medicines reduce the saliva that protects your teeth and gums, including drugs that prevent seizures and that treat a type of chest pain called angina.
- Smoking makes it harder for gum tissue to repair itself.
- Poor oral hygiene habits such as not brushing and flossing every day can lead to gingivitis.
- A family history of dental disease increases your risk of gum disease.
Gum Disease Symptoms
Although the symptoms of periodontal disease could be hard to spot, there usually are warning signs.
The most common symptoms of gum disease include:
- Gums that bleed when you brush your teeth
- Red, swollen gums (healthy gums should be pink and firm)
- Pain or tenderness in the gums
- Bad breath or a bad taste in your mouth that doesn't go away
- Pain when you chew
- Sensitive teeth
- Pus between your teeth
- Gums that pull away from your teeth (receding gums)
- Deep pockets between the teeth and gums
- Loose teeth or teeth that fall out
- Spaces between your teeth that look like black triangles
- Changes in the way your teeth fit together when you bite
In some people, gum disease may affect only certain teeth, such as the molars. Only a dentist or periodontist can tell you for sure that you have gum disease.
Is periodontal disease contagious?
It can be. Bacteria cause gum disease. Those bacteria can pass through saliva if you kiss someone who has gum disease or share utensils with them. You can't catch periodontal disease just from being close to someone.
Gum Disease Diagnosis
A dentist diagnoses gum disease. During a dental exam, the dentist will ask about your symptoms and look for:
- Bleeding, swollen gums
- Pockets between your gums and teeth
- Receding gums
- A change in your bite
- Loose teeth
Your dentist may refer you to a gum specialist called a periodontist for more tests and treatment. The dentist or periodontist uses a small ruler called a periodontal probe to measure the pockets around your teeth. The bigger the pockets, the more bone you've lost. Dental X-rays can show bone loss more clearly.
Gum Disease Treatment
The goals of gum disease treatment are to help your gums reattach to your teeth, reduce swelling, and stop the disease from getting worse. Which treatment plan your dentist or periodontist suggests depends on:
- How severe your gum disease is
- What treatments you've already tried
- How healthy you are
- Whether you smoke
Options include nonsurgical treatments to control bacteria and surgery to fix the tissues that support your teeth.
Nonsurgical treatments
Mild periodontitis can be treated without surgery, using procedures like these:
- Scaling is like a dental cleaning, only it cleans more deeply under your gums. A dental hygienist uses instruments, a laser, or sound waves to remove tartar, plaque, and bacteria from your teeth.
- Root planing smooths out the surface of the root, the part of your tooth that's under your gums. This makes it harder for bacteria and plaque to collect again. It also helps your gums reattach to your teeth.
- Antibiotic mouth rinses, gels, or pills get rid of the bacteria that caused the infection.
Gum disease surgery
If you have advanced periodontitis, you may need one of these surgical procedures:
Flap surgery. This procedure removes plaque that's deep under your gums. Your periodontist makes small cuts in your gum to create a flap. They clean out any bacteria, tartar, and plaque that's under your gums and smooth out any rough spots on the bone. Your gum goes back in place and is closed with stitches. After flap surgery, it will be easier for you to keep your teeth and gums clean.
Soft tissue grafts. The periodontist places gum grafts over spots where your own gums have receded. They take a small piece of tissue from the roof of your mouth or from a donor and attach it to the exposed tooth roots to cover them.
Bone grafting. Periodontitis can wear away the bone around your teeth. This procedure implants pieces of your own bone, artificial material, or donated bone in areas where bone has eroded to hold your tooth in place. In time, your own bone will regrow in that area.
Guided tissue regeneration (GTR). This procedure is often done together with a bone graft. The periodontist puts a special type of fabric between your gums and the bone graft. The fabric holds the space open so that new bone can grow.
Tissue-stimulating proteins. A special protein gel applied to your damaged tooth root helps new, healthy bone and tissue grow.
Platelet-rich fibrin (PRF) and platelet-rich plasma (PRP). PRP and PRF speed healing and reduce pain after gum surgery. Your doctor gets PRF and PRP by spinning a small amount of your blood through a machine called a centrifuge. The machine separates out and condenses a protein called fibrin or a liquid called plasma from your blood. The PRF or PRP then goes onto the surgical site to promote healing.
Can gum disease be reversed?
You can reverse gum disease if you treat it early enough. Once you've lost bone around your teeth, it's not reversible. But you can still slow or stop gum disease with treatment and good oral hygiene.
Gum Disease Prevention
Gingivitis can be reversed and gum disease can be kept from getting worse in nearly all cases when proper plaque control is practiced. Proper plaque control consists of professional cleanings at least twice a year and daily brushing and flossing.
Brush your teeth twice a day. Use a soft-bristled brush and fluoride toothpaste. Replace your toothbrush every 3 months, or sooner if the bristles become frayed. Old, worn-out ones won't clean teeth as well. Brushing gets rid of plaque on the surfaces of the teeth that can be reached.
Flossing removes food particles and plaque from in between the teeth and under the gumline. Floss every day. Don’t wait until something gets stuck between your teeth. Daily flossing gets plaque out of places your toothbrush can't reach. You can also try interdental cleaners, picks, or small brushes that fit in between teeth. Ask your dentist how to use them so you don't damage your gums.
Rinse your mouth. Antibacterial mouthwash not only prevents gingivitis, it fights bad breath and plaque. Antibacterial rinses can reduce bacteria that cause plaque and gum disease, according to the American Dental Association. Ask your dentist which mouthwash would work best for you.
Other health and lifestyle changes can cut the risk of gum disease, lessen how severe it is, and slow how fast it develops. They include:
- Stop smoking. Not only is smoking bad for your heart and lungs, it can harm your teeth and gums. Smokers are seven times more likely to get gum disease than nonsmokers, and smoking can lower the chances of success of some treatments.
- Reduce stress. Stress may make it hard for your body's immune system to fight off infection.
- Maintain a balanced diet. Bacteria in your mouth feed on sugars and starches from food, fueling them to release the acids that attack tooth enamel. Junk food and candy have a lot of extra sugar and starch. Avoid them to keep your teeth and gums healthy. Proper nutrition helps your immune system fight infection. Eating foods with antioxidants – for example, those containing vitamin E (vegetable oils, nuts, green leafy vegetables) and vitamin C (citrus fruits, broccoli, potatoes) – can help your body repair damaged tissue.
- Avoid clenching and grinding your teeth. These actions may put excess force on the supporting tissues of the teeth and could increase the rate at which these tissues are destroyed.
Despite following good oral hygiene practices and making other healthy lifestyle choices, the American Academy of Periodontology says that up to 30% of Americans may be more likely to get gum disease because of their genes. And those who are genetically predisposed may be up to six times more likely to get some form of gum disease. If anyone in your family has gum disease, it may mean that you are at greater risk as well. If you are more likely to have gum disease, your dentist or periodontist may recommend more frequent checkups, cleanings, and treatments to better manage the condition.
If it's been 6 months since you last saw the dentist, set up a cleaning to remove tartar and plaque buildup from your teeth. Ask your dentist about the proper way to brush. Bearing down too hard or missing spots can lead to gingivitis. After a cleaning, your gums should get better within a week or so as long as you brush twice a day, and floss and rinse once a day.
Is Gum Disease Linked to Other Health Problems?
According to the CDC, researchers have uncovered potential links between gum disease and other serious health conditions. In people with a healthy immune system, the bacteria in the mouth that makes its way into the bloodstream is usually harmless. But under certain circumstances, these germs are linked to health problems such as stroke and heart disease. Diabetes is not only a risk factor for gum disease, but gum disease may make diabetes worse.
Takeaways
Gingivitis is the early stage of gum disease. It can lead to periodontal disease and tooth loss. Good oral hygiene and quick treatment can stop gingivitis and help preserve your teeth.
Gum Disease FAQs
What can gum disease lead to?
Late-stage gum disease can lead to tooth loss. Bacteria may also get into your blood and cause coronary artery disease, lung disease, rheumatoid arthritis, poor blood sugar control, and other health problems.
Can I stop gum disease from spreading?
Yes. One way to stop gum disease is to control the infection with nonsurgical or surgical treatments. To keep your teeth and gums healthy, brush and floss regularly to remove plaque.
Can you live a long life with gum disease?
You can have a normal lifespan if you treat gum disease. Uncontrolled gum disease causes inflammation in your body that could shorten your life.

