What Is Osteoarthritis?
Arthritis is a general term that means inflammation of the joints. Osteoarthritis, commonly known as wear and tear arthritis, is the most common type of arthritis. It is associated with a breakdown of cartilage in joints and can occur in almost any joint in the body. It commonly occurs in the weight-bearing joints of the hips, knees, and spine. It also affects the fingers, thumbs, neck, and large toe.
Osteoarthritis -- also called OA -- usually does not affect other joints unless previous injury, excessive stress, or an underlying disorder of cartilage is involved.
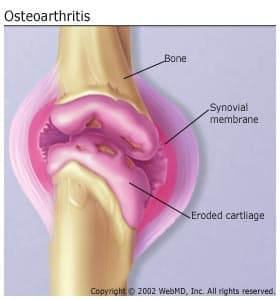
Cartilage is a firm, rubbery material that covers the ends of bones in normal joints. Its main function is to reduce friction in the joints and serve as a "shock absorber." The shock-absorbing quality of normal cartilage comes from its ability to change shape when compressed (flattened or pressed together).
Osteoarthritis causes the cartilage in a joint to become stiff and lose its elasticity, making it more susceptible to damage. Over time, the cartilage may wear away in some areas, greatly decreasing its ability to act as a shock absorber. As the cartilage deteriorates, tendons and ligaments stretch, causing pain. If the condition worsens, the bones could rub against each other.
Types of Osteoarthritis
Your doctor might classify your osteoarthritis as either primary or secondary.
Primary osteoarthritis develops over time. Experts think it's caused by the wear and tear of using your joints throughout your life.
Secondary osteoarthritis is the result of an injury to one of your joints.
Tricompartmental osteoarthritis
This type of osteoarthritis affects your knee. That joint has three compartments: medial, lateral, and patellofemoral. The medial compartment is the side of your knee closest to your other knee. The lateral compartment is the outer side of your knee. The patellofemoral is the front of your knee.
Osteoarthritis can affect any of these compartments. When all three are affected, that's tricompartmental osteoarthritis.
Erosive osteoarthritis
The hand is the joint usually affected by this type, which is also called EOA. EOA is an aggressive form of osteoarthritis that affects what's called the "interphalangeal" joints, the hinges in your fingers that allow you to do things like make a fist. If you have EOA, your affected joints will be swollen, red, and warm. For that reason, it's called inflammatory arthritis. You'll have pain and limited movement. It also can affect the feet and, rarely, hips and shoulders.
Other types of osteoarthritis
Hip. When osteoarthritis affects this joint, you have pain and stiffness in your hip joint. You also might feel it in your groin, butt, or inner thighs. Sometimes the pain can radiate to your knee. As the condition progresses, you'll have less range of motion in your hip.
Spondylosis. This type of osteoarthritis affects your spine. Any part of your spine might be involved. The disks in your back may begin to weaken, and you might get bone spurs – also called osteophytes – on your spine. Nerves in your back might be pinched by weakening disks or bone spurs. As it gets worse, spondylosis can lead to spinal stenosis, a narrowing of the space that your spinal cord and key nerves run through. Depending on what part of your spine is affected, you might have pain or numbness in your shoulders or arms. If the damage is farther down, you may have pain or numbness in your legs.
Shoulder. Osteoarthritis can affect the main joint of your shoulder, the ball-and-socket one known as the glenohumeral joint. A second spot in your shoulder, called the acromioclavicular joint, also can be affected. When that happens, it's called AC joint arthritis. The main sign of this condition is pain in your shoulder, sometimes even when you're not using it. Your shoulder also might be stiff or grind, and you might hear sounds in the joint such as clicking or cracking. That's called crepitus.
Who Gets Osteoarthritis?
Osteoarthritis affects an estimated 32.5 million Americans. The chance of developing the disease increases with age. Most people over age 60 have osteoarthritis to some degree, but its severity varies. Even people in their 20s and 30s can get osteoarthritis, although there is often an underlying reason, such as joint injury or repetitive joint stress from overuse. In people over age 50, more women than men have osteoarthritis.
Osteoarthritis Symptoms
Symptoms of osteoarthritis most often develop gradually and include:
- Joint aching and soreness, especially with movement
- Pain after overuse or after long periods of inactivity
- Stiffness after periods of rest
- Bony enlargements in the middle and end joints of the fingers (which may or may not be painful)
- Joint swelling
Osteoarthritis Causes
Several things can increase your chances of developing osteoarthritis. These include:
Heredity. Some people have an inherited defect in one of the genes responsible for making cartilage. This causes defective cartilage, which leads to more rapid deterioration of joints. People born with joint abnormalities are more likely to develop osteoarthritis, and those born with an abnormality of the spine (such as scoliosis or curvature of the spine) are more likely to develop osteoarthritis of the spine.
Obesity. Carrying extra weight increases the risk for osteoarthritis of the knee, hip, and spine. Maintaining ideal weight or losing excess weight may help prevent osteoarthritis of these areas or decrease the rate of progression.
Injury. Injuries contribute to osteoarthritis. For example, athletes who have knee-related injuries may be at higher risk of developing osteoarthritis of the knee. In addition, people who have had a severe back injury may be more likely to develop osteoarthritis of the spine. People who have had a broken bone near a joint are prone to develop osteoarthritis in that joint.
Joint overuse. Overuse of certain joints increases the risk of osteoarthritis. For example, people in jobs requiring repeated bending of the knee are at increased risk for osteoarthritis of the knee.
Other diseases. People with rheumatoid arthritis, the second most common type of arthritis, are more likely to develop osteoarthritis. In addition, certain rare conditions, such as iron overload or excess growth hormone, increase the chance of developing OA.
Osteoarthritis Diagnosis
The diagnosis of osteoarthritis is based on a combination of the following factors:
- Your description of symptoms
- The location and pattern of pain
- Physical exam
- X-rays
Your doctor may use X-rays to help confirm the diagnosis and make sure you don't have another type of arthritis. X-rays show how much joint damage has occurred. An MRI may be necessary to get a better look at the joint and surrounding tissues if the X-ray results do not clearly point to arthritis or another condition.
Sometimes, your doctor will order blood tests to see if you have a different type of arthritis.
If fluid has accumulated in the joints, your doctor may remove some of the fluid (called joint aspiration) for examination under a microscope to rule out other diseases.
Osteoarthritis vs. rheumatoid arthritis
Osteoarthritis is caused by wear on your joints. Rheumatoid arthritis is an autoimmune disorder. That means your immune system misfires and attacks your joints. The first thing affected is the lining of your joints.
Osteoarthritis Treatment
Osteoarthritis usually is treated by a combination of things, including exercise, weight loss if needed, medications, physical therapy with muscle-strengthening exercises, hot and cold compresses to the painful joint, removal of joint fluid, injection of medications into the joint, and use of supportive devices such as crutches or canes. Surgery may be helpful to relieve pain when other treatment options have not been effective.
The type of treatment will depend on several factors, including your age, activities, occupation, overall health, medical history, location of your osteoarthritis, and severity of the condition.
Osteoarthritis medication
The first step with medication is often over-the-counter pain relievers as needed. These include acetaminophen, ibuprofen, and naproxen. Don't take over-the-counter medications for more than 10 days without checking with your doctor. Taking them longer than that increases the chance of side effects. If over-the-counter treatments aren't effective, your doctor may decide to prescribe a stronger anti-inflammatory drug or other medication to help ease the pain. Some medications in the form of creams, rubs, or sprays may be applied over the skin of affected areas to relieve pain. For some people with persistent pain despite these pills or creams, steroids can be injected directly into the joint. These injections can be given several times a year, though some experts believe this may ultimately speed up joint damage.
Injections of hyaluronic acid directly into the knee joint can relieve pain in some people with osteoarthritis.
When osteoarthritis pain is severe and other treatments are not working, some doctors will give stronger pain pills, such as narcotics.
Unfortunately, none of these will reverse or slow the progression of joint damage caused by osteoarthritis.
Alternative treatments
Although recent research has questioned their usefulness, some medical research has shown that the supplements glucosamine and chondroitin may relieve pain in some people with osteoarthritis, especially in the knee. There is no evidence that glucosamine can help rebuild cartilage. SAM-e (S-adenosyl-L-methionine) is another supplement with potential benefits for osteoarthritis. Some research has shown it may be as effective an anti-inflammatory drugs. SAM-e is a substance found naturally in your body, but it's also available as a supplement. It helps maintain cell membranes. It also helps your body produce and regulate hormones. Remember to let your doctor know about any supplements you're taking because they can have side effects and interact with medications.
Acupuncture has also been shown to provide significant and immediate pain relief in some people with osteoarthritis.
Nutritional supplements that contain avocado and soybean oils – called avocado-soybean unsaponifiables – are used in Europe for knee and hip arthritis. Some studies suggest they can reduce inflammation and slow the damage to your joints.
Omega-3 fatty acids might relieve pain and improve your ability to move. They are found in fatty fish and in fish oil supplements.
Osteoarthritis surgery
When osteoarthritis pain is not controlled with other treatments, or when the pain prevents you from participating in your normal activities, you may want to consider surgery.
There are several types of surgery for osteoarthritis. They include:
Arthroscopy. This procedure cleans out the damaged cartilage or repair tissues. It's most commonly performed on the knee and shoulder. Recent evidence has questioned its effectiveness for osteoarthritis.
Joint replacement. This surgery replaces the damaged joint with an artificial one. Joint replacement surgery should be considered when the severity of the joint pain significantly interferes with your function and quality of life. Even under the best of circumstances, surgery cannot return the joint to its normal state (artificial joints do not have all of the motion of a normal joint), but movement and function are significantly improved. An artificial joint will lessen your pain. The two joints most often replaced are the hip and the knee. Artificial joints are now also available to replace shoulders, fingers, elbows, and ankles to treat severe pain that has not responded to other treatments.
Joint fusion. This procedure removes the damaged joint and fuses the two bones on each side of the joint. This is done more often in areas where joint replacement isn't effective.
Talk to your doctor to see if any of these treatment options are right for you.
Living With Osteoarthritis
You may have to make changes to your daily routine to help you live with your condition.
Exercise and osteoarthritis
Staying at your recommended weight helps prevent osteoarthritis of the knees, hips, and spine, reduces the stress on these weight-bearing joints, and reduces pain in joints already affected. Once you have osteoarthritis, losing weight also can relieve the stress and pain in your knees.
Exercise is important to improve joint movement and to strengthen the muscles that surround the joints. Gentle exercises, such as swimming or walking on flat surfaces, are recommended because they are less stressful on your joints. Avoid activities that increase joint pain, such as jogging or high-impact aerobics. Exercises that strengthen the muscles reduce pain in patients with osteoarthritis, particularly with osteoarthritis of the knee.
Supportive devices
Supportive or assistive devices can help to decrease pressure on the joints with osteoarthritis. Knee supports may be helpful for some people to stabilize the ligaments and tendons and decrease pain. Canes or crutches may be helpful to take pressure off certain joints. If you use a cane, hold it in the hand opposite the joint that hurts.
In addition to pain relief, assistive devices improve function and prevent falls. A licensed physical therapist or other health care professional can recommend which devices are best for you.
There are also many devices to help you perform routine daily activities that may be difficult, such as housework or cooking. Ask your doctor about talking to an occupational therapist to give you ideas about which devices may help. You can find devices that help you grip things and grab them, for instance, if you have arthritis in your hands or wrists.
If you have pain when you stand or walk, you might use inserts for your shoes or braces to make you more comfortable.
Other tips
You may find that exercise such as tai chi or yoga can improve your pain and make you more flexible. Concentrate on slow movement, stretching, and deep breathing. If you take a yoga class, choose a "gentle" course and make sure the instructor knows about your condition. Don't attempt movement that hurts your joints.
Ask your health care provider about self-management education programs in your area. These groups teach skills to cope with your condition. The CDC maintains a website with information about the groups.
Your OA puts you at a higher risk of falls, which can cause broken bones and other injuries. Exercises that focus on strength and balance can reduce your fall risk. You also can make changes in your home to reduce the risk. They include:
- Make sure you have enough lighting. You may need brighter lightbulbs.
- Add grab bars in your bathroom.
- Add railings to both sides of stairs.
- Remove things – such as rugs – that you might trip over.
Takeaways
Osteoarthritis is mostly caused by wear and tear on your joints. It's the most common form of arthritis, and it can affect your knees, hips, hands, wrists, ankles, shoulders, and spine. You're more likely to get osteoarthritis if you have a family history of it, are overweight, put a lot of strain on your joints, or have certain underlying illnesses. There's no cure, but a variety of treatments can ease your symptoms. They include medications and surgical options. You may need to make changes to your daily routine because of osteoarthritis.
Osteoarthritis FAQs
What should you not do with osteoarthritis?
It's important to exercise, but make sure you choose the right type. You may need to avoid:
- Running
- Jumping
- High-impact aerobics
- Tennis
- Anything that requires the same movement over and over, such as a serve in tennis
Don't take over-the-counter pain medication above the recommended dose. If you need more pain relief, talk to your doctor about options.
Don't smoke. The toxins in cigarette smoke can damage your connective tissue.
How do you stop osteoarthritis from progressing?
The best way to stop your condition from getting worse is to focus on a healthy lifestyle. That includes:
- Losing weight
- Managing your blood sugar
- Exercise
- Protecting your joints from further injury
What triggers an osteoarthritis flare-up?
A flare is when your symptoms suddenly get worse. The medicine you've been taking might not be as effective. The main causes of osteoarthritis flares are overusing the affected joint or injuring it. Other causes of flares include:
- Bone spurs
- Repetitive motions
- Weight gain
- Stress
- Infections
- Cold weather
- Changes in barometric pressure

