This year, about 26,500 people in the U.S. will find out that they have stomach cancer, also called gastric cancer, according to the American Cancer Society. That’s lower than in other countries like Japan, China, Chile, and Iceland, which screen for stomach cancer. But the U.S. statistics hold an alarming disparity: Americans of East Asian descent face unusually high risks for stomach cancer.
Why is that, and what can people of East Asian heritage do to help manage that risk?
Here’s what Haejin In, MD, MPH, says. She’s a surgical oncologist at Rutgers Cancer Institute of New Jersey. She specializes in upper gastrointestinal cancers, which includes stomach cancer. She’s also an associate professor of surgery at Robert Wood Johnson Medical School.
Q: In the U.S., how much of a greater risk for stomach cancer do people of East Asian descent face?
A: Koreans are 13 times at risk [compared to White Americans]. Vietnamese are at seven times, and Japanese and Chinese are at five times the risk.
We don’t really have a good understanding of why. We do know that when you look at it globally, it also mimics the exact pattern that we’re seeing in the United States, which is that there are certain countries that have much higher rates of gastric cancer.
Gastric cancer is very prevalent in minorities. The mortality rates for gastric cancer in Blacks, Hispanics, and Asians [are] double of Whites in the United States. It’s a very understudied cancer, especially within Asians and within the minority groups. That research really needs to be done.
Q: Higher rates of Helicobacter pylori (H. pylori) infection in some Asian American groups seem to play a role. How can this infection lead to stomach cancer?
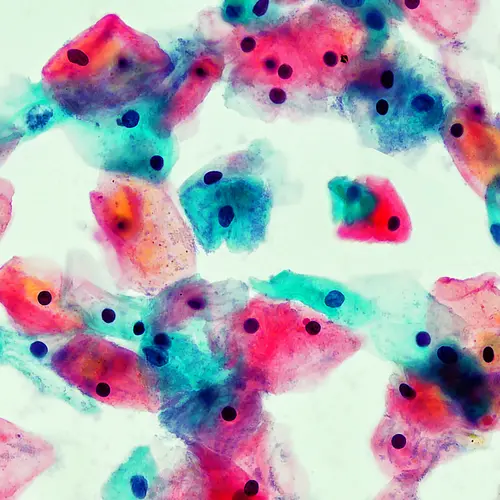
A: Helicobacter pylori is a bacteria that grows in the stomach. At first, it doesn’t cause problems. Then slowly throughout the years, it starts to cause issues, predominantly gastritis. Then later on, it starts to really erode the mucosa [the stomach’s lining], resulting in atrophic gastritis [when your stomach lining has chronic inflammation and thinning] and then the changes that subsequently become gastric cancer.
About the interaction between Helicobacter pylori and diet, there have been studies that have shown that a combination of Helicobacter pylori and a high-salt diet seems to make the risk of gastric cancer higher than either alone.
It's not that all [cases] turn into gastric cancer. We know that only a very, very small percentage of people infected with Helicobacter pylori get cancer. Now, there are also other things that happen with Helicobacter pylori. People get peptic ulcer disease, gastritis – those kinds of things also happen.
Q: Should Asian Americans ask their doctors about getting tested for H. pylori?
A: For most other cancers at rates that high, there are screening guidelines.
A lot of Asians are actually first-generation, and even with the second generation, their risk remains high. As a clinician, I think it makes a lot of sense that people [of East Asian descent] get screened for Helicobacter pylori. It’s just not in the guidelines.
[Testing for Helicobacter pylori done] either through a stool test or a breath test. [If positive,] it’s a 2-week course of antibiotics. That’s pretty much all you need.
Q: Stomach cancer screening programs in Japan and Korea have improved survival rates. Currently, the U.S. has no screening guidelines. What symptoms should prompt Asian Americans to get screened for stomach cancer?
A: The concept of screening is that you’re supposed to do it before you have any symptoms. This is really important because stomach cancer does not have any symptoms until it’s very late. And so screening should really be happening because you are at risk of cancer, not because you’ve developed symptoms for cancer.
Gastric cancer has very vague signs when it develops. Nothing to really point your finger at, but it’s subtle things, like “Oh, it doesn’t quite feel right” or “I’m having some indigestion.” [By the time you’re] losing weight, it’s probably pretty late already.
Don’t wait for symptoms. If you are somebody who has a family history of gastric cancer – either mom, dad, uncles, and aunts – or if you’re from a minority population, particularly the East Asian population, I would advise actually to try to get screened for gastric cancer.
The most proven way of doing it is the way that Japan and Korea are doing it in their population, which is similar to how we think about colonoscopies. [It involves] an endoscopy through the mouth and looking into the stomach. Endoscopy is much easier than a colonoscopy. All you have to do is not eat overnight. You don’t have to bowel-prep or anything like that. It’s a pretty straightforward procedure, taking a quick look to see if anything’s going on and you’re done with your screening.
Q: Is there a takeaway message for doctors?
A: I think, just [have] a very high suspicion of gastric cancer when you’re treating minority populations [and] the fact that Helicobacter pylori and gastric cancer rates are really high. The need for health policies to be developed around this agenda are really pressing [issues] as well.