- Overview
- Causes, Risks & Prevention
- Symptoms & Types
- Tests & Diagnosis
- Your Cancer Care Team
- Treatment & Side Effects
- Treatment Support
- Living With
- Remission & Recurrence
- Support & Resources
- Appointment Prep
- View Full Guide
Guide to Uterine Cancer

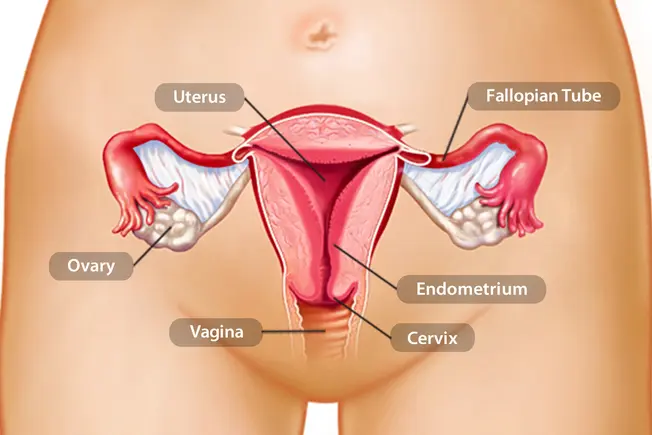
What Is It?
It’s a cancerous tumor in your uterus, the pear-shaped organ also known as your womb. Most cases happen in the lining of the uterus (endometrium), but you can get tumors in the muscles there, too. Over 60,000 women in the U.S. get this type of cancer each year. If you’re past menopause, your chances are higher.

Your Genes
These can play a role in how likely you are to have uterine cancer. For example, Lynch syndrome is a genetic disorder that makes you more likely to get certain cancers. Women with it have much higher odds of getting uterine cancer. But having a problem gene doesn’t mean you’ll get it. It means you and your doctor should watch for signs so you can treat it early if you do. Most women who get uterine cancer don’t have a known genetic cause.

Early Signs
If you haven’t been through menopause and you have bleeding or spotting -- a red, pink, or white discharge -- between periods, see your doctor. The same is true if you’ve had menopause and have these symptoms any time. Bleeding can be a sign of uterine cancer, but it’s also a symptom of other medical problems. Bleeding after menopause isn’t normal, so it definitely needs to be checked out. Your doctor can help you find out what’s going on.

Other Symptoms
Let your doctor know if you have:
- Pain in your pelvis (the area between your hips)
- Lost weight without trying
- Pain during sex
- A hard time peeing or it hurts to pee
It’s best if you find uterine cancer before it grows or spreads, so don’t put off your checkups or ignore symptoms.
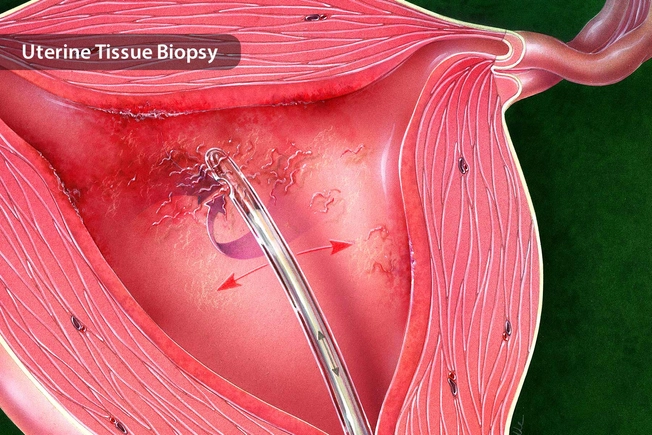
How It’s Diagnosed
You may have an ultrasound so your doctor can see inside your uterus. Your doctor may send a thin, lighted tube in through your vagina to get a closer look. But a biopsy is the best way to know if it’s cancer. Your doctor will take a small amount of tissue from the endometrium and look for cancer cells under a microscope.
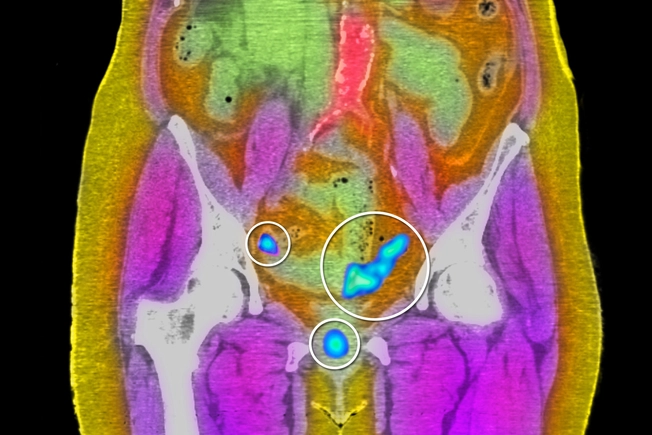
Has It Spread?
If you have uterine cancer, your doctor will start with one of the following to see if it has spread to nearby areas, like your cervix, or to your lymph nodes (tiny glands in your neck, armpits, groin, and other parts of your body):
- Ultrasound
- MRI scan, which uses magnets and radio waves to make detailed images of parts of your body
- CT scan, which takes X-rays from different angles and puts them together to make a more complete picture
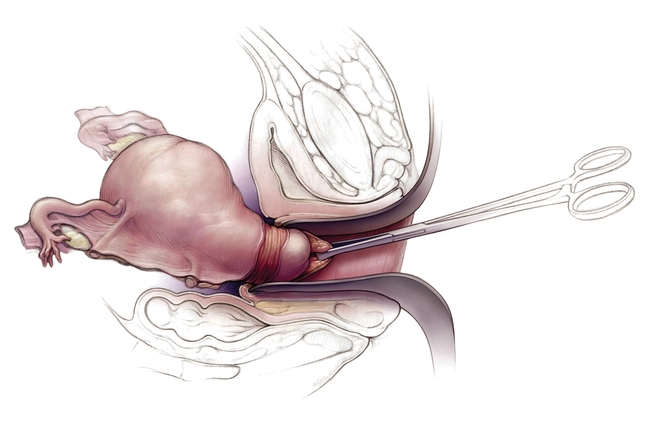
Surgery
Your doctor probably will recommend that your uterus be taken out. They may surgically remove your uterus through your vagina or abdomen. The procedure is called a hysterectomy. Your ovaries and fallopian tubes will probably be removed, too. If your cancer has spread, your doctor also may take out nearby lymph nodes.

Radiation
Your doctor may recommend this after surgery to kill any cancer cells that may still be there. It may also be an option if surgery isn’t a good idea for you. Your doctor may insert a cylinder containing radioactive material into your vagina, or use a machine to aim high-energy rays at the harmful cells. New types of radiation treatment make a 3-dimensional beam that’s the exact shape of the tumor.

Hormone Therapy
Estrogen and other hormones in your body can make uterine cancer grow or spread faster. Drugs like progestins, tamoxifen, LHRH agonists, and aromatase inhibitors are used to block these hormones to slow the tumor’s growth. This can cause side effects that feel like menopause, including hot flashes, weight gain, or dryness in your vagina.

Immunotherapy
These drugs help your own immune system find and attack cancer cells. To keep itself from fighting the body's normal cells, your immune system uses "checkpoints." These are parts of cells that need to be turned on or off to start the disease-fighting process. Drugs that target these checkpoints, called immune checkpoint inhibitors, may help treat some more serious types of endometrial cancer.

Targeted Therapy
Some newer drugs target changes that are seen in cancer cells. Several of them work by stopping new blood vessels from forming in tumors. This helps slow the spread of cancer.

Clinical Trials
You may be able to be part of a test for new and better drugs to treat uterine cancer. Ask your doctor if there are trials in your area and if one might be right for you.

Your Sex Life
Side effects of uterine cancer treatment can change your sex life. Vaginal dryness or mood changes from hormone therapy may make sex painful or reduce your desire. If you’ve had surgery to remove both your ovaries and uterus, you may have the same issues. But lubricants can help with dryness, and some women say their sex lives actually get better after surgery because they have less pain and other symptoms.

Pregnancy
While most women who get uterine cancer are past menopause, younger women can get it, too. If you hope to have children, talk to your doctor about your options, such as storing eggs, before you begin treatment -- surgery, radiation, and hormones can affect your fertility.

Can You Prevent It?
Get regular women’s health checkups so your doctor can spot any signs of cancer early. Your age, genes, and family history may raise your risk of uterine cancer. So can obesity. You can do some things to help prevent it, though, like staying at a healthy weight and getting plenty of exercise. Work closely with your doctor, who can help you control the risk factors that can be controlled.