When you have ulcerative colitis, you want to do whatever you can to keep it from flaring up. So you may be looking for anything that helps, in addition to the medicine and advice your doctor gives you.
Complementary, or integrative, medicine doesn't replace your usual treatments. These are therapies you might try along with your regular medical care.
People in other parts of the world have used some of these methods, like acupuncture, for centuries. But they can be hard for researchers to study. So before you try anything, you should check with your doctor to make sure it won't cause problems with your main treatment or cause side effects.
Mind and Body Techniques
Stress doesn't cause ulcerative colitis. But it can worsen the symptoms and trigger flare-ups. There are several ways you can try to ease it.
Biofeedback. This is a system that teaches you how to control things like muscle tension and rapid heartbeat. At first, a machine helps you recognize what your body is doing. You learn how to quiet the symptoms of stress, and you eventually stop needing the machine.
Deep breathing. You inhale from all the way down, making your tummy expand and pull back in. That helps relax the body, particularly the muscles in your belly. That can be good for your intestines.
Exercise. Physical activity, even if it's mild, can make you feel better and release stress. But if you do too much or make your workout too hard, it might backfire. If you're not active now, ask your doctor what types of exercise would be good to try.
Hypnosis. Sessions with a trained hypnotherapist can help you deal with stress and anxiety. Early research suggests that hypnosis may help relieve the inflammation involved in ulcerative colitis.
Progressive muscle relaxation. You tighten and release various muscle groups, going one group at a time. It's simple to learn, and you can do it anywhere, anytime.
Yoga and meditation. These can help you let go of stress. If you don't have time for a yoga session, you might try even a few minutes of meditation. Just turn your attention to your breath, or to a word or thought that you find calming. Other thoughts will come up. Try to let those go. You might also want to try tai chi, a Chinese martial art known for its slow, meditative movements.
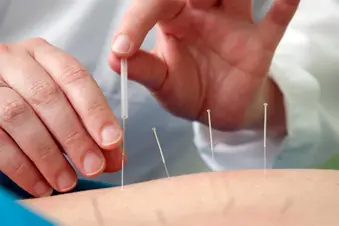
Acupuncture and Moxibustion
Acupuncture is a form of traditional Chinese medicine that places needles in key “acupoints” to ease tension, pain, and other health problems. In moxibustion, practitioners warm and stimulate the same acupoints with burning dried mugwort (moxa) instead of needles. Some studies suggest that these practices can help symptoms of inflammatory bowel disease, like belly pain, nausea, inflammation, diarrhea, constipation, bloating, and gas.
But not all of the studies were exact in the way they collected information, and some studies showed no statistical difference between those who got the treatments and those who didn’t. Some evidence shows that acupuncture can help mood and mental health in people with ulcerative colitis, though more study is needed here as well.
Supplements
There isn't a lot of research that backs using supplements to help manage your ulcerative colitis. These may hold some promise, but the scientific evidence isn't complete, so check with your doctor first:
Aloe vera. It might help ease inflammation. But it could give you diarrhea.
Fish oil. This also might ease inflammation, and it may help in combination with prescription drugs from a group called aminosalicylates, though more studies are needed.
Psyllium. This comes from the ground seeds of the psyllium plant, and it supplies fiber. If you have diarrhea because of ulcerative colitis, it may help. But too much of it might cause irritation. For some people, fiber from flaxseed or oat bran may work better. Psyllium can interfere with some medications.
Turmeric. This spice contains a chemical called curcumin. When combined with standard treatments for UC, it may have some benefits, but more research is needed.
Probiotics
These are “good” bacteria that live in your digestive system and help it work. The research on whether they help your body handle ulcerative colitis isn't certain.
Some studies have found no benefit. But others showed that a particular probiotic called VSL #3 may do some good in addition to your regular medical treatment. There's also some research showing that a drink that includes fermented milk and another probiotic, bifidobacteria, may also help in addition to ordinary treatment.
Finally, if you're curious about going to a chiropractor to help with pain, ask your doctor what they think. It might be fine to try, but as usual, it's best to let your medical team know so they have a complete picture of your health.
Show Sources
(Photo Credit: Stockbyte/Getty Images
SOURCES:
Alimentary Pharmacology and Therapeutics: “Review article: Complementary and alternative therapies for inflammatory bowel disease.”
Mayo Clinic: “Osteopathic medicine,” “Ulcerative colitis,” “Acupuncture,” “Diagnosis.”
The Journal of the American Osteopathic Association: “Osteopathic Primary Care of Patients with Inflammatory Bowel Disease: A Review.”
Natural Medicines Comprehensive Database.
American College of Gastroenterology: “Ulcerative colitis.”
Canadian Society of Intestinal Research: “Worms and Inflammatory Bowel Disease.”
Canadian Journal of Gastroenterology: “Exercise and inflammatory bowel disease.”
Crohn's and Colitis Foundation: “Acupuncture in Inflammatory Bowel Disease,” “Inflammatory Bowel Disease and Irritable Bowel Syndrome: Similarities and Differences.”
National Center for Complementary and Integrative Health: “Meditation: In Depth,” “Relaxation Techniques for Health.”
Gastroenterology and Hepatology: “Acupuncture in Inflammatory Bowel Disease.”