Unexpected Places You Can Get Skin Cancer


Under a Fingernail
This “subungual melanoma” might happen under a toenail too. The thumb and big toe are the most common areas, but it’s possible under any nail. It’s not usually due to sun exposure, but past injuries could be a cause. If you notice a dark streak under the nail for no apparent reason, see your dermatologist.

Soles of the Feet
It’s often the same type of cancer, acral lentiginous melanoma, that can form under your fingernails. Asians and African-Americans get it more often than any other melanoma. It typically starts as a flat dark patch that is clearly distinct from the skin around it, but it may sometimes be reddish or orange in color. You’ll likely get surgery to remove the cancer and may follow up with radiation, chemotherapy, or biologic immunotherapy.

Palms of the Hands
If you have darker skin, melanoma is more likely in body areas that don’t get much sun, such as the palms of the hands and soles of the feet. And acral lentiginous melanoma in particular is far more likely in people with darker skin colors. Only about 2% of cases happen in light-skinned people. It’s often more serious than other melanomas, in part because people often don’t notice it until it’s far along and harder to treat.

Eyelid
Too much sun is often the cause of this type of skin cancer. You can get it surgically removed, and it’s usually not serious if treated early. The cancer starts most often in the basal cells in the upper layer of skin (epidermis). A more serious form starts in the squamous cells, which are even closer to the surface of your skin. This type grows more quickly and spreads more easily to nearby tissues.

Scalp
It’s common to have growths or tumors on your scalp, but they’re often not cancer. In fact, only about 13% of total skin cancers are on the scalp, usually the less serious “nonmelanoma” cancers like basal cell and squamous cell carcinoma. Talk to your doctor if you have a sore on your head. If it’s cancer, it may be a small, smooth, waxy lump that may bleed or get crusty. But you need to see your doctor to find out.
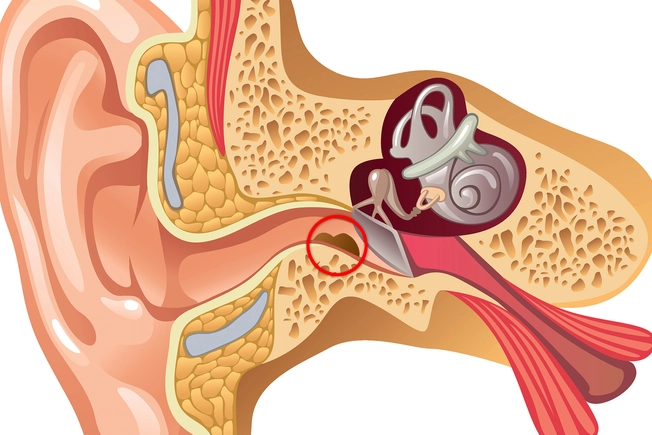
Inside Your Ear
Left untreated, skin cancer on the outside of the ear (squamous or basal cell) can spread to the inside of your ear. This includes the ear canal that runs from your outer ear to the tiny bones in your middle ear to the hair-like nerves in your inner ear that send signals to your brain, and the temporal bone that encases it all.

Tongue
You might notice flat, hard, white patches (leukoplakia) that you can’t scrape off, or tingling, loss of feeling, or a lump or sore that won’t go away. It’s typically squamous cell. And it’s much more likely if you use tobacco or drink a lot, and especially if you do both. Your doctor might take some cells from the suspicious area to look at under a microscope (biopsy). You’d usually get surgery to remove it.

Lip
Nonmelanoma cancers, often basal or squamous cell, are the ones that typically affect your lips. Your lower lip is about 12 times more likely to get it than your upper lip, which doesn’t get as much sun. Men also get cancer here more often than women, perhaps because men tend to use tobacco and alcohol more. Your risk also rises if you have the human papillomavirus virus (HPV) that can cause warts on your genitals, hands, or elsewhere.
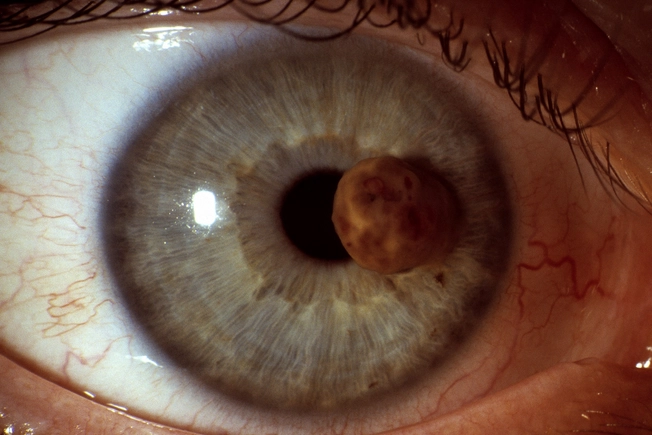
Iris
You might see “uveal” or “intraocular” melanoma as a dark spot in the colored iris around your pupil. You also might get blurry or spotty vision. Skin cells called melanocytes grow out of control and form a tumor. It’s the most common form of cancer that starts in the eye, and it can spread to other parts of your body through your lymph nodes. It also could spread to other parts of your body, usually the liver, through your bloodstream.
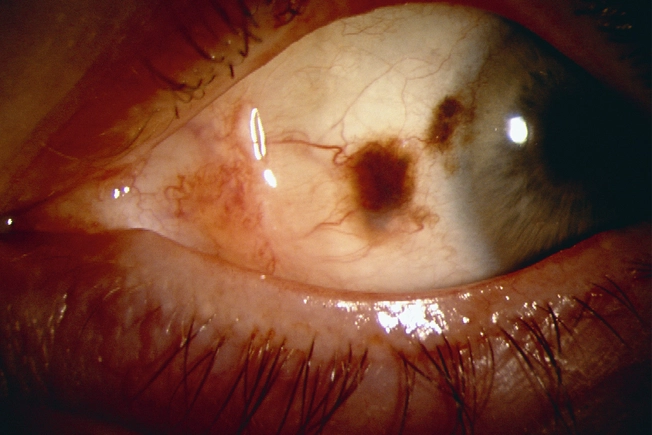
White of Your Eye
Conjunctival melanoma is a cancerous growth on the conjunctiva, the clear membrane that covers the surface of the eye and inner eyelid. It often appears as a dark or red spot in the white of your eye. It can be serious and may spread to other parts of the body through the lymph nodes or bloodstream. If your doctor suspects it, they might take a sample of the tissue to look at under a microscope to help determine if it’s cancer.

Prevention: Know Your Risk
Talk to your doctor about any family history of skin cancer. Other things that raise your risk for sun damage and cancer include:
- Light skin, hair, or eyes
- Freckles or moles that are large, numerous, or oddly shaped
- Lots of time outside, especially at higher altitude or where it’s very hot
- Illness or medication that weakens your immune system
- Drugs that make your skin more sensitive to light

Prevention: Check Your Skin
Skin cancer is often curable if you find it early. So it’s important to check your skin once a month or so. Stand in front of a full-length mirror to start. A chair and a hand mirror can help you get a view of awkward places. Look for any new growths or changes in old spots, as they may be a sign of problems, including cancer. See a skin doctor (dermatologist) once a year or anytime you notice something unusual.