Why Your Feet Hurt


Your Shoes
High heels, for example, put more pressure on the balls of your feet, which can thin your foot’s natural padding where you need it most. Avoid heels higher than 2 1/4 inches when you’re going to do a lot of walking. Flip-flops and overly pointed or flexible shoes also could lead to foot pain. You can avoid this if you match the shoe to the activity and make sure of proper fit and support.

Arthritis
Many types of arthritis affect your feet. Osteoarthritis, the most common, happens when cartilage breaks down and allows bone to rub against bone. Gout causes uric acid crystals to build up in your big toe and leads to pain and swelling. In rheumatoid arthritis, lupus, and other autoimmune disorders, your body’s immune system attacks the joints in your feet and ankles, causing inflammation.

Bunion
Your doctor might call it hallux valgus. This painful, bony lump grows at the joint where your big toe meets your foot. It happens slowly over time as your big toe pushes inward. Bunions often run in families. Tight, narrow, shoes like high heels don’t cause them, but they can make them worse. Ice, special pads, and roomy footwear can all help. Your doctor might suggest surgery in serious cases.

Bursitis
Bursae are small fluid-filled sacs that cushion joints, bones, and tendons. But repeated motion or friction from shoes can inflame them. In your foot, this most often happens in the toes and the heel, which might get red, swollen, and painful. Ice, padding, and over-the-counter pain meds like acetaminophen and ibuprofen can help. For a serious case, your doctor might suggest a corticosteroid injection or even surgery.
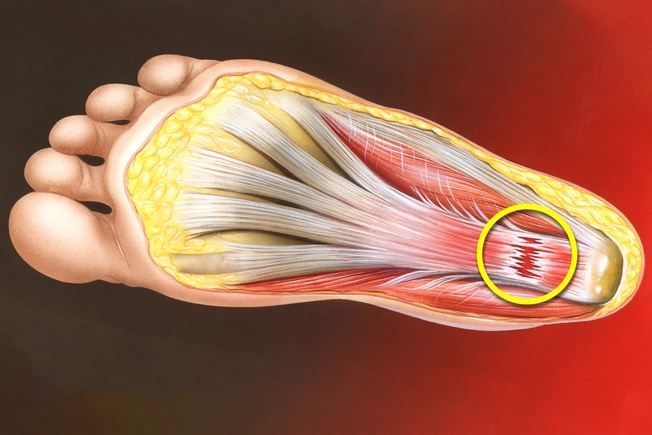
Plantar Fasciitis
This common cause of heel pain involves the ligament that connects the front and back of your foot and supports your arch. It isn’t always clear why it gets swollen and irritated, but you’re more likely to get it if you have high arches or tight calves. It can also result from repeated impact on your feet, like running, or when you start a new activity.

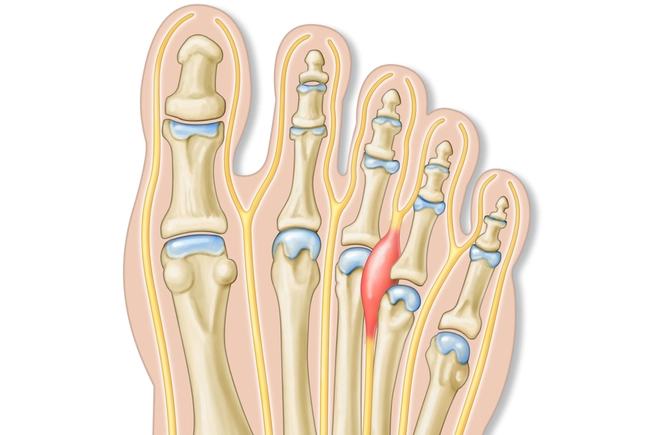
Stress Fracture
Pounding your feet over and over, as in running, basketball, tennis, and other sports, can cause tiny cracks in your metatarsals -- the long bones just below your toes. Once this happens, you’ll notice swelling and pain with any type of activity that caused the injury. Rest for 6-8 weeks to give it a chance to heal. If you don’t, you might create more serious damage that’s harder to treat.

Sprains and Strains
Sprains pull, twist, or tear the ligaments that connect your bones to each other, often when you fall or get hit. Strains are the same type of damage to the tendons that connect muscles to bone. Aside from the most common spot, the ankle, you can also get them in the middle of your foot, around the arch, or at the base of your big toe. The area may become swollen and bruised, and it’ll probably be hard to walk. Treat it with RICE -- rest, ice, compression, elevation -- for the first 2 days. Talk to your doctor if it still hurts after 2 weeks.

Broken Bone
Your foot is made up of many small bones. It’s easy to break one of them when you fall, in an accident, or while you’re playing sports. Your foot will likely hurt and get swollen and bruised. The shape around the break, whether toe or instep, may not look right. The doctor will try to get your bone straight again and keep it still with a cast so it can heal. A severe break might require surgery.
Morton’s Neuroma
This might be to blame if you have pain in the front part of your foot or feel like you’re walking on a rock or a marble. It happens when tissue around a nerve starts to thicken. It can affect any toe, but it’s common between your third and fourth toes. Women get it far more often than men, likely because they tend to wear shoes with tapered toes and high heels that squeeze their feet. Your doctor will likely suggest rest, ice, padding, and over-the-counter pain medicine. If these treatments don’t help, you might need surgery.
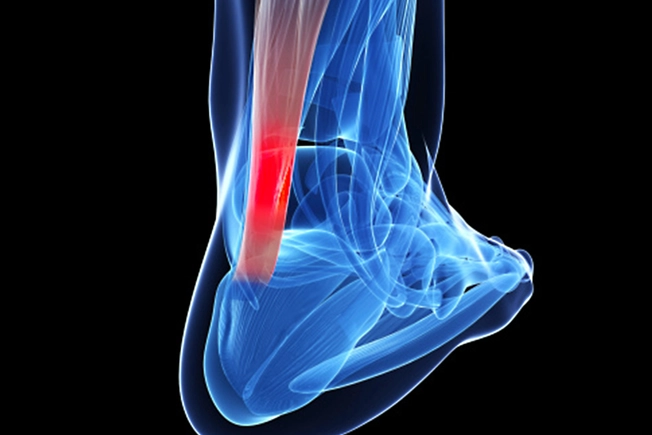
Achilles Problems
The Achilles is a thick tendon that connects your calf muscles to your heel. Repeated motion can inflame it (your doctor will call it tendinitis). A jump or fall, often during sports, can tear or rupture it. You might hear a sudden pop and feel a sharp pain in the back of your lower leg. Your heel could swell, and it may hurt to stand on your toes. Rest and icing are important for both. You doctor might suggest surgery in serious cases.

Plantar Warts
These growths often show up on weight-bearing areas like your heel and the balls of your feet. They happen when the human papilloma virus (HPV) gets into your body through a break or cut in the skin. The skin may feel thick, painful, and tender. They usually go away on their own without treatment, but you can try over-the-counter remedies if it lingers. Talk to your doctor if you can’t get rid of the warts.

Peripheral Neuropathy
This results from damage to the nerves that connect your spinal cord to your feet. It might start with numbness and tingling and progress to jabbing pain. Diabetes is the most common cause, but others include cancer drugs (chemotherapy), kidney failure, autoimmune diseases like rheumatoid arthritis, toxic chemicals, infection, and nutrition problems.

Tarsal Tunnel Syndrome
Your tibial nerve goes through this tunnel between your ankle bone and a group of ligaments near the top of your foot. The nerve helps you feel on the bottom of the foot. Swelling from injury, arthritis, bone spurs, fallen arches, or other conditions could push on the nerve. You might have shooting pain, numbness, and a tingling or burning feeling in your foot.

Raynaud’s Phenomenon
This condition causes blood vessels in your hands or feet overreact to cold or stress. During an attack, they narrow and limit blood supply. This can make your toes cold and numb. They could even turn white or blue. As blood returns, they may start to tingle and hurt. Medication can help symptoms and prevent tissue damage.