Primary idiopathic hypersomnia (IH) is a rare sleep disorder that causes extreme tiredness during the day for no clear reason. The word “idiopathic” means there’s no known cause, and “hypersomnia” means excessive sleep.
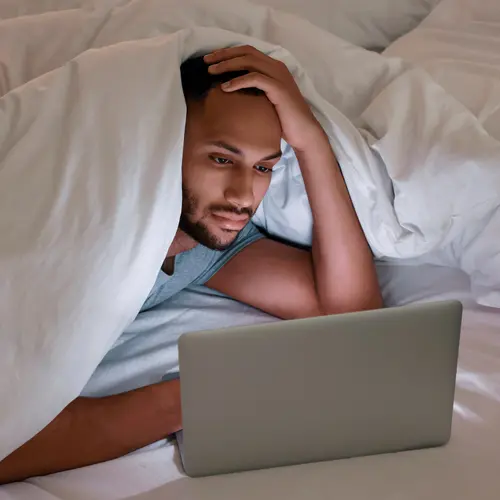
When you have idiopathic hypersomnia, the urge to sleep can happen anytime, even if you get plenty of sleep at night. You may not be able to stay awake and alert throughout the day. It can negatively affect your social life, work life, and home life.
Experts aren’t sure exactly how many people live with IH. Researchers estimate that about 5% of the population has it.
What Causes It?
Primary IH happens on its own, which means it’s not triggered by other medical conditions.
Though the exact cause isn’t known, research has suggested the sleepiness may be due to:
- A brain chemical abnormality. Some people with IH have too much of a small molecule in their cerebrospinal fluid (fluid that surrounds the brain). This molecule interacts with GABA, which is a brain chemical that promotes sleep.
- Genes. Up to 39% of people with IH have a family history of the disorder.
There also seems to be a link between IH and psychiatric conditions, like depression, anxiety, or psychosis.
It’s possible that IH may have many causes, not just one.
What Are the Symptoms?
IH can cause symptoms that may develop slowly. Some of these are:
- Excessive daytime sleepiness
- Trouble staying awake throughout the day
- Sleeping enough hours during the night but still feeling tired
- Taking long naps during the day
- A hard time waking up in the morning or after naps
- Feeling confused, groggy, or unrefreshed when waking up
- Anxiety or crankiness
- Low energy
- Restlessness
- Slowed thinking or speech
- Problems with memory, focus, or concentration
- Headaches
- Loss of appetite
- Dizziness or lightheadedness when standing
- Hallucinations (You see, hear, or smell things that aren’t there.)
People with IH typically sleep for at least 11 hours each day, but still feel tired. Sometimes, the need to sleep can strike while you are driving a car or at other dangerous times.
Diagnosis and Testing
It can be difficult to diagnose IH. You may get a diagnosis if:
- You have had symptoms of IH for at least 3 months.
- Your symptoms are severe and affect your daily life.
Your doctor will likely ask about your medical history, symptoms, sleeping habits, and medications. You may need to keep a sleep diary to log your patterns. Also, your doctor might ask you to wear a special sensor on your wrist to track your sleep-wake cycles for several weeks.
Some tests that might help doctors diagnose IH are:
- Polysomnography. This is an overnight sleep study that measures your breathing patterns, brain waves, eye movements, and other body functions while you sleep.
- Multiple sleep latency test. It’s a daytime sleep test that measures the types and stages of your sleep while you nap.
- Sleep questionnaire. Your doctor may ask you to rate your sleepiness with a tool, such as the Epworth Sleepiness Scale.
Questions for Your Doctor
When you see your doctor, it’s a good idea to bring a list of questions.
You can ask:
- What could be the cause of my sleepiness?
- What treatments do you recommend?
- Do these treatments have side effects?
- What kind of results can I expect?
- What should I do if I feel sleepy while I drive?
- What else can I do to stay more alert during the day?
Treatment Plan
Since they don’t know the cause, doctors typically aim to treat the symptoms of IH.
Some medications that may be useful are:
- Wakefulness-promoting drugs. Armodafinil (Nuvigil), modafinil (Provigil), pitolisant (Wakix), or solriamfetol (Sunosi).
- Psychostimulants. Amphetamine, dextroamphetamine (Dexedrine, ProCentra, Zenzedi), or methylphenidate (Concerta, Daytrana, Methylin, Ritalin).
- Other meds. Clarithromycin (Biaxin), flumazenil (Romazicon), or sodium oxybate (Xyrem).
In 2021, the drug Xywav, which contains lower-sodium oxybate, was approved by the FDA for IH in adults. It’s thought to affect brain chemicals while you sleep, which may help with daytime symptoms. But Xywav has a high potential for misuse or abuse.
Your doctor might also suggest that you make lifestyle changes. For instance, you may want to keep a regular sleep schedule and limit caffeine and alcohol before bedtime.
How the Condition Might Change Over Time
IH usually develops gradually. This means your symptoms might start out mild but slowly become more severe as time goes on.
Tips for Living With It
It can be hard to live with IH. Here are some ways to help you feel more alert:
- Go to bed at the same time each night.
- Keep your bedroom cool, dark, and quiet.
- Avoid alcohol, tobacco, caffeine, and exercise before bed.
- Be careful when you drive or operate equipment that can be dangerous.
- Avoid night shift work.
What to Expect
IH is a chronic illness without a cure. It’s not life-threatening, but IH can affect your well-being. Treatments and certain lifestyle changes can help improve your symptoms, but some people don’t find complete relief.
Taking Care of Yourself
Along with good sleep hygiene, try to eat a healthy diet and exercise regularly. Physical activity can improve sleep and give you more energy. Just remember not to exercise too late in the day.
How to Get the Support You Need
Along with the physical toll it takes, IH can drain you emotionally, too. Your loved ones might not understand your constant need to sleep. A mental health professional can help you manage your feelings. Usually, your doctor or sleep specialist can refer you to someone who fits your needs.
Support groups are also an option for people with IH. These groups allow you to connect with other people who have the same condition.