1 of 5 / Overview
View All
What Is Heart Disease?
You asked. We answer. Here's an easy-to-read, illustrated guide to heart disease.
Men and Heart Disease
When you think of heart disease in men, usually people think of coronary artery disease and heart attack.
Women and Heart Disease
Heart disease is the leading cause of death in women over 40 years old, especially after menopause.
What Causes Heart Disease?
Most heart attacks are the end result of coronary heart disease, a condition that clogs coronary arteries with fatty, calcified plaques.
2 of 5 / Symptoms & Types
View All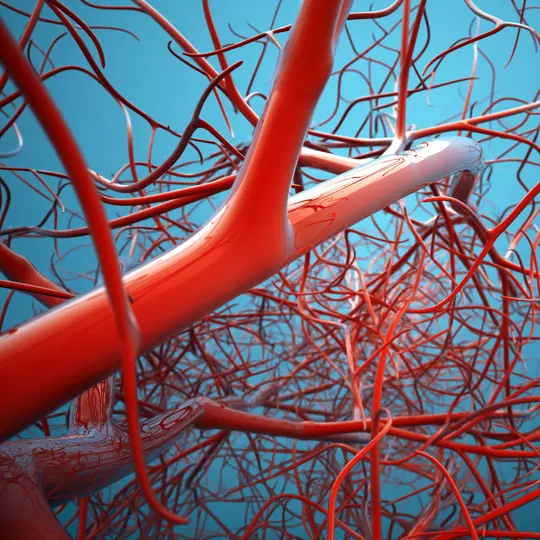
Heart Disease Warning Signs
Here's a fast, easy-to-understand guide to the symptoms of each type of heart disease.
Enlarged Heart (Cardiomegaly)
An enlarged heart (cardiomegaly) can have various causes. But it's usually caused by hypertension or coronary artery disease.
Irregular Heart Rhythm
Irregular heart rhythm -- arrhythmia -- is when your heart doesn't keep up a good beat. Learn what it means here.
Heart Valve Disease
You may not know what a heart valve is -- until it stops working right. It's a common form of heart disease.
3 of 5 / Tests & Diagnosis
View All
Echocardiogram
There are several variations on the echocardiogram, or "echo." Learn about these ultrasound-like tests of the heart.
Chest X-Ray
Why get a chest X-ray? What happens? Click here for quick answers.
Stress Test
Does your heart respond well to exertion? That's what a stress test looks for. Here's a straightforward description.
Tilt Table Test
The head-up tilt table test is used to help find the cause of fainting spells. Here's what you need to know.
4 of 5 / Treatment
View All
Stents
Get information about why they’re used and what types are available.
Heart Bypass Surgery
If you need to have bypass surgery, you’ll have lots of questions about how it works and how it can help.
Valve Disease Treatment
When your heart valve disease needs attention, it can be treated by traditional surgery or by balloon valvuloplasty.
Pacemakers
A pacemaker is a small device that sends electrical impulses to the heart muscle to keep up a suitable heart rate and rhythm.
5 of 5 / Living With
View All
After a Heart Attack
Here are steps you can take after a heart attack to ensure a full recovery.
Cardiac Rehab
It's very likely your doctor will encourage you to get involved in a cardiac rehab program.
Heart-Healthy Cooking
Got heart disease? Nothing is more important than eating heart-friendly foods. See what heart-healthy cooking is all about.
Safe Exercises for Heart Disease
What exercises are best for those diagnosed with heart disease? Read more.
Suggested Reads about Heart Disease
Heart-Liver Surgery May Help Patients Excluded from Transplant List
Patients with both heart and liver diseases are usually turned away from organ transplant lists. A new dual procedure aims to give them another chance.
This Heart Attack Hits Young Women, But Doctors Often Unaware
SCAD accounts for 1 in 3 acute heart events in younger women. Many doctors are not aware it exists.
Lower-Income Americans at Higher Risk of Death From Excess Salt
Lower-income communities often have less access to fresh, healthy food, leaving convenience stores and fast food as the primary sources of food.
Fasting Study Under Fire After Heart Conference
Early research has suggested that if you have heart disease, intermittent fasting may raise the risk of death from heart disease, drawing skepticism from experts and cautions from the researchers themselves.
8 million+ Physician Ratings & Reviews
Find Doctors and Dentists Near You
You can also search by physician, practice, or hospital name