Throughout our lives, healthy cells in our bodies divide and replace themselves in a controlled fashion. Cancer starts when a cell is somehow altered so that it multiplies out of control. A tumor is a mass composed of a cluster of such abnormal cells.
Most cancers form tumors, but not all tumors are cancerous.
Benign, or noncancerous, tumors do not spread to other parts of the body, and do not create new tumors. Malignant, or cancerous, tumors crowd out healthy cells, interfere with body functions, and draw nutrients from body tissues.
Cancers continue to grow and spread by direct extension or through a process called metastasis, whereby the malignant cells travel through the lymphatic or blood vessels -- eventually forming new tumors in other parts of the body.
The term "cancer" encompasses more than 100 diseases affecting nearly every part of the body, and all are potentially life-threatening.
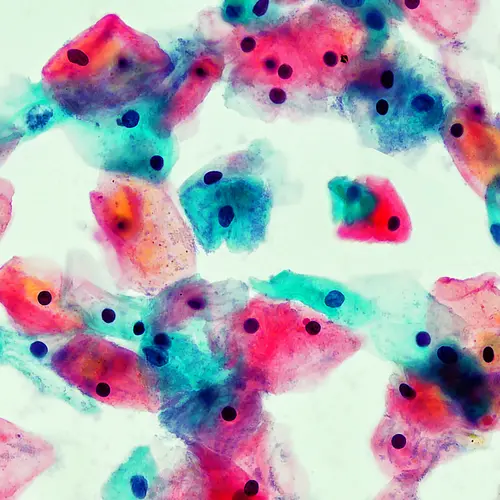
The major types of cancer are carcinoma, sarcoma, melanoma, lymphoma, and leukemia. Carcinomas -- the most commonly diagnosed cancers -- originate in the skin, lungs, breasts, pancreas, and other organs and glands. Lymphomas are cancers of lymphocytes. Leukemia is cancer of the blood. It does not usually form solid tumors. Sarcomas arise in bone, muscle, fat, blood vessels, cartilage, or other soft or connective tissues of the body. They are relatively uncommon. Melanomas are cancers that arise in the cells that make the pigment in skin.
Cancer has been recognized for thousands of years as a human ailment, yet only in the past century has medical science understood what cancer really is and how it progresses. Cancer specialists, called oncologists, have made remarkable advances in cancer diagnosis, prevention, and treatment. Today, more people diagnosed with cancer are living longer. However, some forms of the disease remain frustratingly difficult to treat. Modern treatment can significantly improve quality of life and may extend survival.