What Is Vulvar Cancer?
Vulvar cancer is when cancerous cells grow out of control on or in the vulva, the outer part of a woman’s genitals. It’s different from vaginal cancer, which starts inside the vagina.
A woman’s vulva includes:
- The opening of the vagina. This is the tubelike channel that leads out from their uterus.
- The labia. These are two sets of skin folds that look like lips. The labia majora are the fleshy set on the outside. The labia minora are thinner and set inside them.
- The clitoris. This is a sensitive knob of tissue under a hood of skin where the labia minora meet.
- The mons pubis. This is the soft mound in front of their pubic bones that becomes covered with hair in puberty.
- The perineum. This is the patch of skin between their vulva and anus.
Vulvar Cancer Symptoms
You might not notice any symptoms early on. Over time, you might have:
- A change in the color of your vulva
- Unusual growths or bumps that may be red, pink, or white and feel rough or thick
- A change in how a mole looks
- Thickened skin on your vulva
- An open sore
- Itching that doesn’t go away
- Pain, soreness, or burning
- Unusual vaginal bleeding or discharge
- Pain when you pee
These can also be signs of other conditions, so talk to your doctor if you spot problems.
Types of Vulvar Cancer
There are several main forms of this disease.
Squamous cell carcinoma. This is the most common type. It starts in your skin cells. It might be linked to the human papillomavirus (HPV), especially in younger women. A subtype called verrucous carcinoma grows slowly and can look like a wart.
Adenocarcinoma.This type usually starts in cells in the Bartholin’s glands just inside the opening of your vagina. This is also called Bartholin gland cancer. It can look like a cyst. It also can form in sweat glands in the skin of your vulva or in the top layer of vulvar skin, which is called Paget’s disease.
Melanoma.This type forms in cells that make pigment, or skin color. You’re more likely to get it on skin that’s exposed to the sun, but it sometimes forms on your vulva.
Sarcoma. This starts in bone, muscle, or connective tissue cells. It can happen at any age, including in childhood.
Basal cell carcinoma.This is the most common type of skin cancer. It usually appears on skin that’s exposed to the sun, rarely on the vulva.
Vulvar Cancer Causes and Risk Factors
The exact causes of vulvar cancer aren’t clear. But certain things can raise your chances of getting it. These include:
- Age. More than half of cases are in women over age 70.
- A history of unusual Pap tests
- HIV or AIDS
- HPV
- Melanoma or unusual moles
- A family history of melanoma
- A precancerous condition like vulvar intraepithelial neoplasia (VIN). These are changes in cells or tissue that can happen years before you’re diagnosed with cancer.
- Vaginal or cervical cancer
- Lichen sclerosus, a condition that makes vulvar skin thin and itchy
- Smoking, especially if you’ve also had HPV
Vulvar Cancer Diagnosis
Your appointment might include:
- A medical history. Your doctor will ask about your overall health, including habits and illnesses.
- A pelvic exam. They’ll check your vulva for signs of cancer by looking at the area and feeling your uterus, vagina, ovaries, bladder, and rectum.
- Colposcopy. A magnifying tool called a colposcope can give a close-up look at any problem areas in your vagina, vulva, and cervix. This procedure is also called a vulvoscopy.
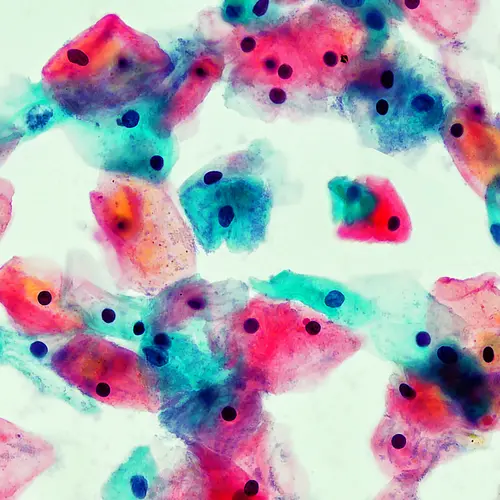
- Biopsy. Your doctor might take a bit of tissue for a specialist to look at under a microscope.
- Imaging tests. X-rays, CT and PET scans, and MRIs make detailed pictures of the inside of your body to tell your doctor if you have cancer or how far it’s spread.
Vulvar Cancer Stages
If tests show signs of cancer, your doctor will look at how big the tumor is and whether it’s spread. This is called staging.
- Stage I. The tumor is small and hasn’t spread past your vulva and perineum.
- Stage II. The cancer has moved into nearby tissues but not your lymph nodes.
- Stage III. It’s spread to nearby tissues and to the lymph nodes in your groin.
- Stage IV. Cancer has reached the upper part of your vagina, urethra, or anus, or a part of your body that’s farther away.
Vulvar Cancer Treatment
Treatment depends on many things, including the type of cancer, how far it’s spread, and your overall health. The four main treatments are:
- Surgery. This is the most common. Your doctor might use one of these procedures:
- Ultrasound surgical aspiration. Sound waves break up the tumor into small pieces, and your doctor takes them out.
- Laser surgery. They use a laser to cut into or take out affected tissue such as your lymph nodes, parts of your vulva, or other organs. This treatment is not used for invasive tumors.
- Excision. Your doctor takes out the tumor and tissue around it.
- A wide local excision removes some of the tissue.
- A radical local excision takes out a large amount of tissue and possibly lymph nodes.
- Vulvectomy. Part or all of your vulva is removed. There are several types:
- Skinning vulvectomy. Your doctor takes the top layer of skin off your vulva.
- Simple vulvectomy. This procedure removes your entire vulva and tissue just under the skin.
- Partial or modified radical vulvectomy. This involves removing most of your vulva and possibly nearby lymph nodes.
- Radical vulvectomy. Your doctor removes the entire vulva and nearby lymph nodes.
- Pelvic exenteration. This procedure removes your vulva and lymph nodes as well as one or more of the nearby organs: your lower colon, rectum, bladder, uterus, cervix, or vagina.
- Radiation therapy. This uses high-powered X-rays or other forms of radiation to kill cancer. Your doctor might use a machine that beams the rays into your body or implant a radioactive needle or seed inside your body, on or near the cancer.
- Chemotherapy (“chemo”). This uses medicines to kill or stop the growth of cancer cells. You can take these drugs by mouth or through an IV. Some kinds come as a lotion or cream that you put on your skin.
- Biologic therapy, or immunotherapy. This targets your immune system to boost your body’s defenses against cancer.
Vulvar Cancer Outlook
After treatment, you’ll see your doctor often for follow-ups. You may need to have pelvic exams every 3 to 6 months for 2 years, and then every 6 to 12 months for 3 to 5 years. Your doctor might also recommend more screening tests.
Your results will depend on the type of cancer and its stage. Overall, more than 70% of women who have vulvar cancer live at least 5 years after they’re diagnosed.
The 5-year survival rate is 86% for women whose cancer hasn’t spread beyond their vulva. If it’s spread to nearby tissues or lymph nodes, the rate is 53%. Of women whose cancer has spread farther in their body, about 23% live 5 more years.
Experts estimate that 1,350 women in the United States die of vulvar cancer each year.
Side effects of vulvar cancer treatment
Before you start treatment, talk to your doctor about what to expect, including possible side effects.
Wound problems are common after vulvar surgery. It’s important to keep the area clean and practice good hygiene.
Surgery, radiation, or chemo can also cause:
- Irritation or damage to your bowels or bladder. This may lead to changes in your bathroom habits, but they often go away within a few weeks.
- Scarring, dryness, and shrinking of tissue in your vagina
- Discomfort when wearing tight pants
- Urinary infections
- Fluid-filled cysts near the wound
- Blood clots that can travel to your lungs
- Severe swelling in your legs because of a buildup of lymphatic fluid (lymphedema)
- An opening between your bladder or rectum and vagina (fistula)
Keep your medical team updated on any treatment side effects so they can help you manage them.
Vulvar cancer and sex
It’s common to have some sexual and psychological issues after treatment for vulvar cancer. Your body might look or feel different. You could have pain during sex and a hard time reaching orgasm or even peeing.
Don’t hesitate to talk to your medical team about these changes and what steps you can take. Counseling can help, or you might choose to have reconstructive surgery.
Vulvar Cancer Prevention
You can lower your risk of vulvar cancer with a few lifestyle changes:
- Avoid HPV. Limit your number of sex partners. Practice safe sex, including using condoms. Get the HPV vaccine, which can help prevent genital warts and several kinds of cancer.
- Don’t smoke.
- Get regular checkups. Talk to your doctor as soon as possible if you notice a problem between visits.