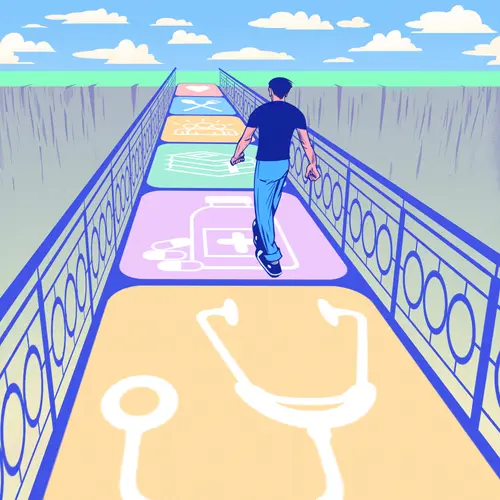
Nov. 7, 2023 – People with depression, anxiety, or long-term stress have a higher risk of heart problems, two new studies show. The findings are more evidence of the mind-heart connection, showing how poor brain health can open pathways to cardiovascular disease, which is the top cause of death in the nation.
In one of the new studies, researchers found that people diagnosed with depression or anxiety developed risk factors for major heart problems 6 months earlier than people who didn’t have depression or anxiety. (Risk factors included developing high blood pressure, type 2 diabetes, and high cholesterol.)
Overall, people in the study who had depression or anxiety had a 35% higher risk of a major cardiovascular event, such as a heart attack or stroke. The faster development of health conditions like high blood pressure came from the higher risks caused by depression or anxiety, eventually leading to the heart or stroke events, the researchers said.
The team from Massachusetts General Hospital evaluated 10 years of health data for 71,262 adults whose average age was 49 years old. In addition to looking at the start of risk conditions like type 2 diabetes and outright cardiovascular diagnoses, they explored how a genetic trait known to make people sensitive to stress affected heart health.
People who had the genetic risk for stress developed their first risk factor for heart problems an average of 1.5 years sooner, compared to people who didn’t have the genetic tendency for stress.
The study, along with a second separate project that evaluated stress and heart health, will be presented this weekend at the American Heart Association’s Scientific Sessions 2023 in Philadelphia.
The findings “suggest that depression and anxiety might induce brain changes that trigger downstream effects in the body, such as increased inflammation and fat deposition,” according to a research summary from the conference organizers.
The results could lead to calls for more frequent screenings among people with depression or anxiety to see if they have conditions like high blood pressure, high cholesterol, and type 2 diabetes, so that the high-risk conditions can be identified and treated earlier.
Cardiovascular disease, which refers to heart disease and conditions that affect blood vessels, is the leading cause of the death in the U.S., killing more than 800,000 people per year, federal health data shows. More than 1 in 10 adults in the U.S. have been diagnosed with heart disease.
In a second study that will also be presented at the conference, researchers found that cumulative stress had an impact on brain and heart health. Higher cumulative stress carried a 22% higher risk of a condition called atherosclerosis, in which plaque builds up in the arteries, reducing blood flow. Cumulative stress also was linked to a 20% higher risk of cardiovascular disease, including coronary artery disease and heart failure.
High levels of cumulative stress were most common among:
- Women
- People ages 18 to 45 years old who also had lower income and education levels
- Black and Hispanic people
- People who experienced racial or ethnic discrimination
- People who lacked health insurance
- People who had high blood pressure, were overweight, were physically inactive, or smoked
The researchers said stress directly affected physical health and also led to unhealthy lifestyle habits, such as smoking or being sedentary, all of which led to higher health risks. The findings build upon previous knowledge of the mind-heart connection, which have shown that high stress hormones like cortisol can affect blood sugar, inflammation, and other biological responses that affect the heart.
The people in the study filled out questionnaires as part of the Dallas Heart Study, and none of the 2,685 people had cardiovascular disease at the start of the study. The questionnaire responses were used to get a numerical score of what the researchers called “perceived stress.”
“There is indeed a mind-heart connection. Taking care of your mind can impact your physical health as well,” lead author of the cumulative stress study Ijeoma Eleazu, MD, a cardiology fellow at the University of Texas Southwestern Medical Center in Dallas, said in a statement. “It would be great to see more patients talking with their physicians about their stress levels and more physicians screening for a high burden of stress in their patients. In that way, we can work together to combat poor outcomes.”