- Headaches Overview
- Migraine
- Cluster & Tension Headaches
- Other Types of Headaches
- Appointment Prep
- View Full Guide
All About Headaches


When Your Head Aches
Your pain may be constant or throbbing, and it may get worse over time or not. But one thing is certain: When you have a headache, it’s hard to think about anything else. The more you know about each type, and which ones affect you, the better you can manage them.
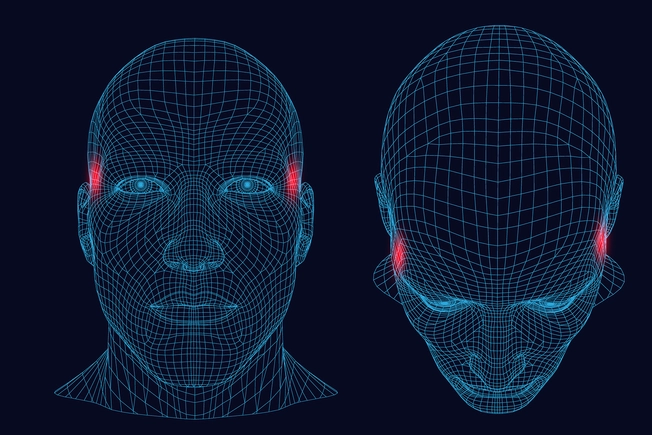
Tension Headaches
Also called muscle contraction or stress headaches, these are the most common kind of headache. The pain is usually on both sides, and you may feel as if a belt is tightened on your head or something is pushing on your face, head, or neck. You also may be more sensitive to light and sound.

Tension Headaches: Causes
Physical postures that strain your head and neck muscles -- like when you hunch over a computer for hours or pin your phone to your ear with your shoulder -- can cause these headaches. Stress, intense work, missed meals, depression, anxiety, and too little sleep can affect the muscles in your neck, face, scalp, and jaw, and lead to them, too.

Tension Headaches: Treatment
If a health issue -- like arthritis, teeth grinding, or sleep apnea -- is causing them, your doctor will treat that first. If that doesn’t help or you don’t have other problems, they might suggest an over-the-counter medication like acetaminophen or ibuprofen. A hot shower or putting a warm washcloth on the back of your neck might help. If those don’t work, you might try meditation or another relaxation technique to manage your stress.
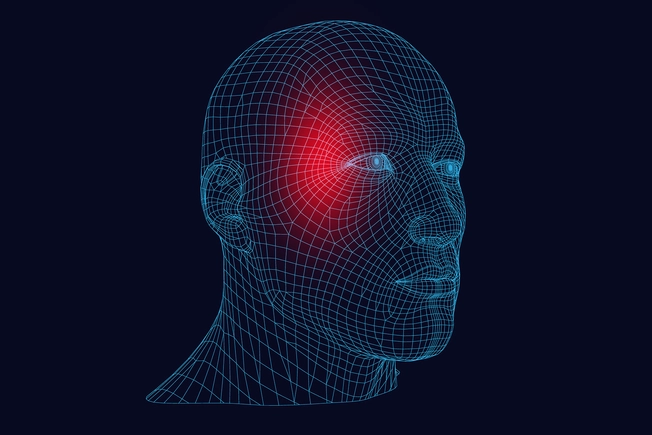
Migraines
Throbbing pain builds, typically on one side of your head. It can be intense, and talking or walking can worsen it. You might be nauseated and sensitive to light, noise, and smells. Food cravings or changes in how much you pee can happen the day before a migraine. Some people also have an “aura” before, during, or after one. You could smell strange odors, have ringing in your ears, see flashing lights or wavy lines, or have blind spots.

Migraines: Triggers
There are different theories about why some people get them and others don’t, but genetics and the environment may play roles. Hormonal changes, stress, sleep problems, strong odors, tobacco, missed meals, flashing lights, and anxiety are among the things that can trigger them. And certain foods and drinks can, too. Coffee, wine, aged cheeses, pickled foods, pepperoni, and salami are just some of the possibilities.

Migraines: Treatment
It’s best to rest with your eyes closed in a quiet, dark room with something cool on your forehead. Drink lots of fluid, especially if you’re vomiting. Your doctor may prescribe drugs, either to prevent migraines or ease your symptoms. But using these too often can lead to “rebound” headaches, so follow your doctor’s instructions. You may also be prescribed the use of a noninvasive nerve stimulation device to help relieve migraine symptoms. You also might keep a journal of what you do or eat the day before a migraine to figure out your triggers.
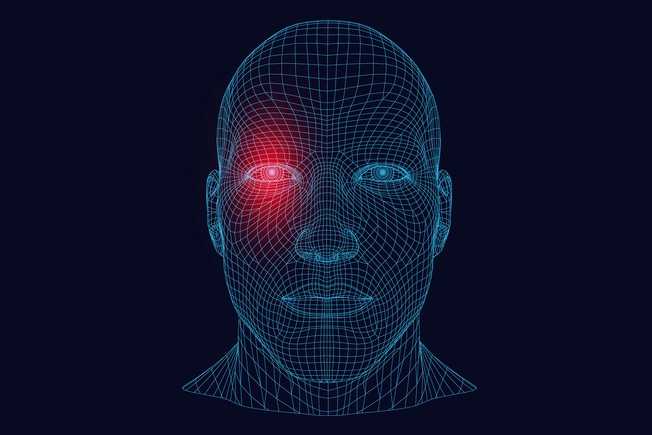
Cluster Headaches
These are sudden, very painful headaches on one side of your head, often behind one eye. They usually happen at the same time of day for several weeks. The pain typically is worst 5 to 10 minutes after it starts and can last 3 hours. Your nose and eye may redden and swell on the side where the pain is, and you may be sensitive to light, sound, or smell. You might have an aura (like with a migraine) and feel nauseated beforehand.

Cluster Headaches: Causes
Because they’re more likely to happen at night, some doctors think they might be caused by irregular sleep. Alcohol -- especially red wine -- and smoking may also be triggers, and your chances of getting them are higher if they run in your family or you’ve had some kind of head injury. They happen more often in the spring and fall, and they're sometimes mistaken for allergies.

Cluster Headaches: Treatment
Your doctor may suggest a kind of therapy where you breathe pure oxygen to make less blood flow to your brain. Researchers aren’t sure exactly why, but studies show that this can help most people who get cluster headaches. They may also prescribe triptan drugs -- also used for migraines -- that narrow blood vessels and ease pain. In more serious cases, a noninvasive nerve stimulation device or surgery is used to stop the signals to and from certain nerves.
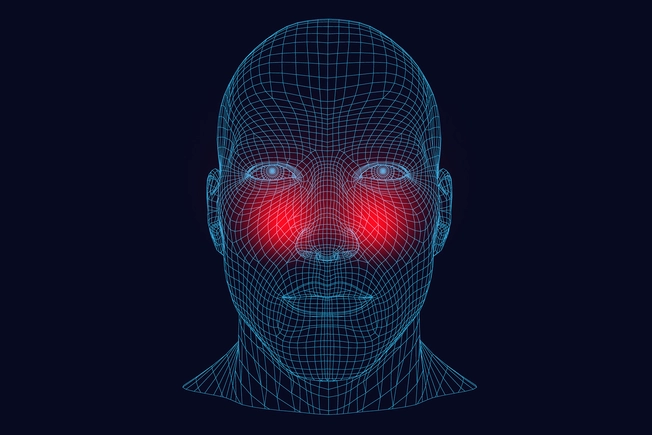
Sinus Headaches
Most people who think they have these actually have migraines. With both types, you can have pain in your face, nasal congestion, and watery eyes, and both may get worse when you lean forward. But a sinus infection, which brings on sinus headaches, also causes thick, yellow mucus, and you might have a fever and trouble smelling, too. You don’t have those symptoms with migraines.

Sinus Headaches: Treatment
A sinus infection usually gets better on its own within a week or so. If it lasts longer, you may have a bacterial infection and need antibiotics. Your doctor also may suggest you clear your sinuses with a saline solution, or they might give you corticosteroids to help with inflammation. When the infection is gone, your headache should be, too.
Secondary Headaches
This kind is brought on by an illness or condition that affects your brain. A sinus headache is an example, because it’s caused by an infection. Other conditions that can cause headaches include concussions, a problem with your blood vessels, brain tumors, and seizures.

Secondary Headaches: Treatment
Your doctor will work with you to figure out what’s causing them and how to treat that condition. Once you’ve taken care of the other problem, your headache should get better.
IMAGES PROVIDED BY:
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
- Getty Images
SOURCES:
American Migraine Foundation: “Sinus Headaches.”
Cleveland Clinic: “Migraine Headaches.”
Mayo Clinic: “Sinus Headaches: Symptoms,” “Sinus Infections -- Most Clear Up without Antibiotics,” “Chronic Sinusitis.”
National Headache Foundation: “Oxygen Therapy.”
National Institutes of Health: “Meninges,” “Headache: Hope Through Research.”