For most people, relapsing and remitting MS (RRMS) turns into secondary progressive MS (SPMS) at some point. The usual pattern of relapses and remissions starts to change. You may have fewer relapses or none at all. But your MS symptoms will gradually get worse. These changes happen slowly, so you and your doctor might not notice them at first.
How long does it take for RRMS to become SPMS?
No one knows exactly, but it could take as long as 20 to 25 years. Because SPMS is so complex, doctors usually wait at least 6 months to diagnose it.
How will I know it's SPMS?
The shift to SPMS isn't easy to spot. You might start to notice some changes in your MS. But if you still have relapses, it can be hard to tell if it's SPMS or not.
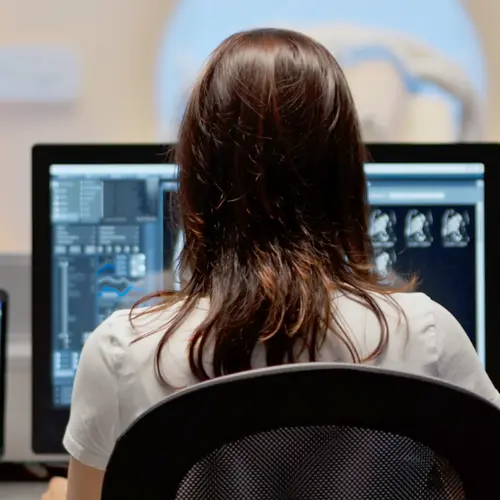
Your doctor can diagnose SPMS based on your symptoms over time, a neurological exam, and MRI scans.
Why did I get SMPS?
SMPS is the second stage of RRMS, and it happens to almost everyone.
A disease-modifying medicine, like interferon beta, for RRMS can make relapses happen less often and make your symptoms less severe. But it probably won't stop RRMS from turning into SPMS.
Are there different types of SPMS?
You may have heard about active and inactive SPMS, or SPMS with progression and without progression.
When SPMS is active, your symptoms flare or you might even have new ones. When it's inactive, things are quiet.
SPMS with progression means your MS is getting worse, maybe faster than before. This could show up on a test, or you might notice it yourself.
It's important to know what SPMS is doing so you and your doctor can decide on the right treatment at the right time.
Will I still be able to take care of myself?
Like other types of MS, SPMS varies a lot from person to person. You have more disability with SPMS, but how fast that happens or what it will be like is hard to say. You may have times when your symptoms get a little better and times when they stay the same.
One way to think about SPMS is that you may be able to do many of the things you did before but in new ways. For instance, you may need a cane or walker to help you walk. Or, you might need a wheelchair to get around.
This doesn't mean you can't take care of yourself or have an independent life.
Do I need a rehab team?
You and your doctor should work together to find the support you need when you first learn you have MS. Rehab specialists like physical and occupational therapists can ease many of your symptoms so you can feel better and get around better. These people can help when you have trouble with everyday activities, like dressing and driving, or problems with your speech or memory.
Will my treatment plan change?
If you still have relapses, you're likely to keep taking the same medicine you took for RRMS. If it stops working, your doctor may switch to a different disease-modifying medicine. These drugs only help with relapses, though. They don't slow or stop SPMS.
Your doctor can prescribe medicine to ease other symptoms you may have, like bladder problems or depression.
Are there medications to treat SPMS?
The FDA has approved a medicine for SPMS called cladribine (Mavenclad), mitoxantrone (Novantrone), ofatumumab (Kesimpta), ponesimod (Ponvory), and siponimod (Mayzent). Mitoxantrone can have serious side effects, like infections, heart disease, and a type of cancer called leukemia. Doctors do not prescribe it that often as a result.
What other options do I have?
A healthy lifestyle plays a big part in your treatment.
Regular exercise can relieve fatigue, help with strength and balance, make your gut and bladder work better, and lift your mood. Try to choose something that gets your heart pumping, like swimming or brisk walking. If those are too tough, check out tai chi. It's a form of gentle movement anyone can do.
Eating fruits, veggies, fish, and healthy fats is good for you overall and may lower your chances of disability and depression. Not so good are red meat, starches, sugar, and processed foods.
Supplements like vitamin D, vitamin B12, and lipoic acid are generally safe and could help slow worsening symptoms. Talk to your doctor about taking them.
What about medical marijuana?
Some people with MS use marijuana for pain and other symptoms. And many who don't use it say they might give it a try.
Not much is known about how marijuana helps MS. But it's been shown to safely ease pain and muscle spasms that can make it hard to walk or speak. If you live in a state with medical marijuana, you can ask your doctor if it may help you.