What Are Pressure Sores?
You may know pressure sores by their more common name: bedsores. Also sometimes called pressure ulcers, they happen when you lie or sit in one position too long and the weight of your body against the surface of the bed or chair cuts off blood supply. You might get them if you're on bed rest or in a wheelchair.
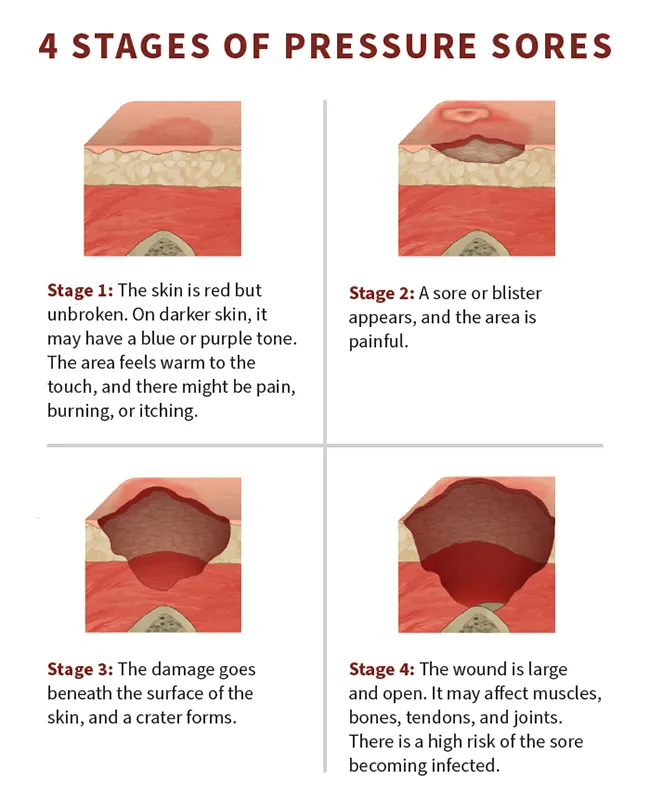
Your doctor may talk about the "stage" of your pressure sores. The stages are based on how deep the sores are, which can affect how they're treated.
If found early, there's a good chance these sores will heal in a few days, with little fuss or pain. Without treatment, they can get worse.
Pressure Sores Causes
Pressure sores happen when your skin is pressed against a surface (like a mattress or a cushion) for a long period. This makes it hard for blood flow to reach that area of skin. As a result, skin cells begin to die, and the area becomes sensitive. Pressure sores can show up in a few days or even just a few hours.
A few things contribute to pressure sores:
Pressure. Even if it doesn't feel like you're putting a lot of weight on a certain body part, over time, the force adds up. The pressure squeezes your skin, making it hard for blood to flow through that area. Without proper blood flow, your skin can't get enough oxygen or nutrients. This weakens the skin and causes cells to die.
Rubbing. Rubbing, even from blankets or clothing, can damage sensitive skin. This could be especially harmful if the skin is moist from sweat.
Stretched skin. When two surfaces slide against each other, it can cause your skin to pull or stretch. For instance, you might slide down a raised bed, aggravating the skin on your tailbone.
Common areas of pressure ulcers
Pressure sores tend to form in bony parts of your body, like the skin covering your spine and tailbone. These places don't have a lot of fat or muscle padding. The places where you get them depend on your position.
If you spend most of your time in bed, you're most likely to find them on your:
- Head (where it rests against the pillow)
- Shoulder blades
- Hips
- Tailbone and butt
- Back of the knees
- Ankles
- Heels
If you stay in a wheelchair for long periods, you might get them on your:
- Shoulder blades
- Spine
- Arms or legs (where they touch the chair)
You also can get pressure sores from devices that press against your skin for long periods. For example, wearing an oxygen mask can lead to pressure sores on your nose, your ears, or the back of your head. Oral devices (like poor-fitting dentures) can cause sores in your mouth.
Pressure Sores Risk Factors
Some people are more likely to get pressure sores than others. Things that can raise your risk of pressure sores include:
- Immobility. This is when you have difficulty moving. You might spend a lot of time in a position that puts pressure on a certain body part.
- Incontinence. This is when you can't control your bladder or bowels. Moisture from pee and poop could irritate your skin, especially if you're not able to clean up right away.
- Poor nutrition and hydration. Your skin (and the rest of your body) needs a healthy diet with plenty of nutrients and water. Without these, it will get weak and fragile.
- Loss of physical feeling. Pain, discomfort, and other sensations tell your body when it's time to shift position. Some health conditions, like spinal cord injuries, can dull your ability to feel. As a result, you might not realize when pressure builds up on a certain body part.
- Blood flow problems. Some conditions, like diabetes and vascular disease, make it hard for blood to travel throughout your body. This raises the risk that certain positions might cut off your blood flow, causing pressure sores.
- Thin or weakened skin. Wearing a cast or prosthetic device could cause your skin to weaken. This makes your skin more vulnerable to pressure and irritation.
What health conditions raise your risk of bedsores?
Certain diseases make it hard to move or get out of bed. They might cause immobility, blood flow problems, and other things that raise your risk of pressure sores. These conditions include:
- Cancer
- Cerebral palsy
- Coma
- Dementia
- Diabetes
- Heart failure
- Kidney failure
- Malnutrition
- Paralysis
- Spinal cord injury or spina bifida
- Vascular problems
Pressure Sores Stages and Symptoms
There are four stages of pressure sores from mild to severe:
Stage I
This is the mildest stage. These pressure sores only affect the upper layer of your skin.
Symptoms: Pain, burning, or itching are common symptoms. The spot may also feel different from the surrounding skin: firmer or softer, warmer or cooler.
You may notice a red area on your skin. If you have darker skin, the discolored area may be harder to see. The spot doesn't get lighter when you press on it or even 10-30 minutes after you stop pressing. This means less blood is getting to the area.
Stage II
This happens when the sore digs deeper below the surface of your skin.
Symptoms: Your skin is broken, has an open wound, or looks like a pus-filled blister. The skin around it may be discolored.
The area is swollen, warm, and/or red. The sore may ooze clear fluid or pus. And it's painful.
Stage III
These sores have gone through the second layer of skin into the fat tissue.
Symptoms: The sore looks like a crater and may have a bad odor. It may show signs of infection: red edges, pus, odor, heat, and/or drainage. The tissue in or around the sore is black if it has died.
Stage IV
These sores are the most serious. Some may even go so deep they affect your muscles, ligaments, and bones.
Symptoms: The sore is deep and big. Skin has turned black and shows signs of infection—red edges, pus, odor, heat, and/or drainage. You may be able to see tendons, muscles, and bone.
Other stages
In addition to the four main stages for bed sores, there are two others:
Unstageable is when you can't see the bottom of the sore because it's covered in a layer of dead skin. Your doctor can only stage it once it's cleaned out.
Suspected deep tissue injury is when the surface of the skin looks like a stage I or II sore, but underneath the surface, it's a stage III or IV sore.
Pressure Sores Diagnosis
To diagnose a pressure sore, your doctor will examine your skin. They might ask questions like:
- When did the sore appear?
- Does it hurt?
- How often do you change positions?
- Have you ever had a pressure sore before?
Your doctor will consider your symptoms. Then they'll determine whether you have a pressure sore, and if so, what stage it's in. They might take a picture to record its healing progress.
If your doctor is worried you might have an infection, they might do:
- Blood tests
- Biopsies to take a sample of tissue for testing
- Imaging, such as an X-ray or MRI, to get a picture of what's happening under your skin
Pressure Sores Complications
When left untreated, pressure sores can lead to other problems such as:
Skin infections. Open wounds can let bacteria in and lead to bacterial infections like cellulitis or septicemia. You might notice the area becoming warm, swollen, and inflamed.
Sepsis. If left untreated, infections can lead to sepsis, when your body starts to attack its own tissues instead of fighting the bacteria causing the infection.
Amputation. Sepsis can be so bad that you have to have a limb removed.
- Bacteria in your bloodstream. This can lead to serious problems like bacterial meningitis or endocarditis. These diseases affect the brain and heart.
Bone and joint infections. Pressure sores can allow infections to enter nearby bones or joints. These kinds of infections can damage tissues and affect your ability to move.
Cancer. Rarely, wounds that take a very long time to heal can turn into a type of skin cancer called squamous cell carcinoma.
Signs of an infected bedsore
Infection can cause:
- Fluid leaking from the sore
- Fever
- Bad smell
- Warm skin near the wound
- Changes in skin color
- Swelling
- Pain
Pressure Sores Treatment
How you treat a pressure sore depends on what stage it's in.
Stage I
The first and most important thing to do with any pressure sore is to stop the pressure. Change your position or use foam pads, pillows, or mattresses.
If you spend a lot of time in bed, try to move at least once every 2 hours. If you're sitting, move every 15 minutes. You may need someone to help you.
Wash the sore with mild soap and water and dry it gently.
It may help to eat a diet high in protein, vitamins A and C, and the minerals iron and zinc. These are all good for your skin. Also, drink plenty of water.
Stage II
Clean the wound with a saline (saltwater) solution and dry it gently. Keep the sore covered with a bandage. Ask your doctor what type is best—films, gauze, gel, foam, or medicated.
If you see signs of an infection, such as pus, fever, or redness, tell your doctor.
Stage III
Stage III sores will need more care, so you should see your doctor. They may remove any dead tissue. This is called debridement. They'll numb the surrounding skin first, then use a scalpel to remove the dead skin or special ointments to dissolve it.
Your doctor also might prescribe antibiotics to fight infection. You may also be able to get a special bed or mattress through your insurance.
Stage IV
Tell your doctor right away. These wounds need immediate attention, and you may need surgery.
Pressure sore medications
Pressure sores can be painful. To help with the pain, you can try nonsteroidal anti-inflammatory drugs like ibuprofen (Advil) and naproxen sodium (Aleve). Take them before changing positions or cleaning your wound. Your doctor could also prescribe pain relievers in the form of a cream or ointment.
If your bedsore becomes infected, you might need prescription antibiotics.
Pressure sore surgical treatments
If you have a large pressure sore that doesn't go away, you might need a surgery called a skin graft. The surgeon takes muscle or skin from a different part of your body and uses it to cover the sore. This closes the wound and cushions it.
Pressure Sores Prevention
There are some easy ways to prevent pressure sores. The most important one is to regularly change positions. Here are some tips:
Reposition yourself often. Move around every 15 minutes (if you're in a wheelchair) or every hour (if you're in bed). Don't be afraid to ask for help.
Get a specialized wheelchair. Look for chairs that you can tilt back, allowing you to shift your weight more easily.
Use cushions. Cushions and specialized mattresses can help distribute your weight, relieving pressure. They also can support your body in comfortable positions. But don't use doughnut cushions—these actually build pressure on the surrounding area.
Keep the head of your bed low. Don't raise the head of your bed (or tilt your pillows) to more than a 30° angle. This prevents you from sliding down the bed, which could strain the skin surrounding the tailbone.
If possible, lift yourself. If you're in a wheelchair and have enough upper body strength, you can do wheelchair pushups. This is when you press your forearms against the arms of the chair to lift your body from the seat.
Other ways to prevent pressure sores include:
Stay clean and dry. Even if you can't bathe regularly, use a daily cleansing towel to wipe away sweat, dirt, and other buildup. Pat dry when done. If you have incontinence, apply a moisture barrier ointment. This will protect your skin from pee and poop.
Avoid irritating the skin. Look for buttons, zippers, bumps in the fabric, and other things that could cause rubbing. Wash your blankets and clothes frequently.
Eat a healthy diet and drink plenty of water. Staying well-nourished and hydrated will help your skin stay strong.
Keep an eye on your skin. Check yourself (or ask someone else to check) for signs of bedsores. The earlier you treat them, the quicker they will go away.
Pressure Sores Prognosis
How quickly bedsores heal depends on how serious they are. In general, healing can take a few weeks or months. Usually, bedsores get better after treatment and don't cause any long-term problems, although your skin might be a little weaker in that area. But some severe sores might need surgery.
Takeaways
Bedsores form when you lie or sit in one position for a long time. They can be mild to severe, depending on how long you've had them. To avoid them, change positions often (you might need someone to help you). Talk with your doctor about preventing and treating infected sores.
Pressure Sores FAQs
How do you get rid of pressure sores?
How you treat a pressure sore depends on its severity. Generally, you'll need to avoid putting pressure on that area and clean it regularly. More serious bedsores might need antibiotics (if they're infected) or surgery.
What does a stage I pressure sore look like?
During this early stage, your skin in the area of the sore may be red. It may also feel different to the touch than the rest of your skin—firmer or softer, or cooler or warmer.
What does a stage II pressure sore look like?
These pressure sores might cause broken skin, blistering, and pus.
What is the cause of pressure sores?
Pressure sores develop when an area of your skin experiences pressure, rubbing, or stretching for a long period.

